Colonoscopy
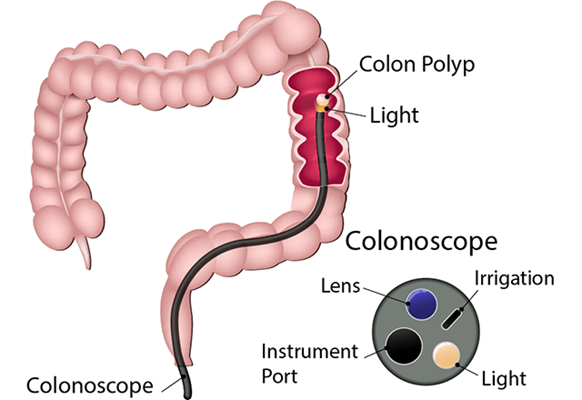
A colonoscopy is a procedure that lets your health care provider check the inside of your entire colon (large intestine).
The procedure is done using a long, flexible tube called a colonoscope. The tube has a light and a tiny camera on one end. It is put in your rectum and moved into your colon.
In addition to letting your provider see the inside of your colon, the tube can be used to:
- Clean the lining of your colon using irrigation (a water jet)
- Remove any liquid stool with a suction device
- Inject air into your bowel to make it easier to see inside
- Work inside your bowel with surgical tools
During a colonoscopy, your provider may remove tissue or polyps (abnormal growths) for further examination. He or she may also be able to treat problems that are found.
Anatomy of the Colon
The colon is the last section of your digestive system. It absorbs water to change waste from liquid to solid stool. The large intestine is about 5 feet long in adults. It has the following four sections:
- Ascending colon: extends upward on the right side of your belly
- Transverse colon: extends from the ascending colon across your body to the left side
- Descending colon: extends from the transverse colon downward on your left side
- Sigmoid colon: extends from the descending colon to your rectum
The rectum joins the anus, which is the opening where stool passes out of your body.
Why might I need a colonoscopy?
Colonoscopy can help your provider look for problems in your colon. These include any early signs of cancer, inflamed (red or swollen) tissue, ulcers (open sores) and bleeding.
Cancer Screening
Colonoscopy is also used to screen for colon cancer and rectal cancer. Screening involves looking for cancer in individuals who do not have any symptoms of the disease.
Colonoscopy can also be used to check the colon after cancer treatment.
Checking and Treating Problems
A colonoscopy may be used to check and, if needed, treat problems such as:
- Colon polyps
- Tumors
- Ulcerations
- Inflammation
- Diverticula (pouches) along the colon wall
- Narrowed areas (strictures) of the colon
- Any objects that might be in the colon
It may also be used to find the cause of unexplained, chronic (long-term) diarrhea or bleeding in the gastrointestinal (GI) tract.
Results of Other Tests
Colonoscopy may be used when other tests show the need for additional testing. These include the following:
- Barium enema
- Computed tomography (CT) colonography (also called virtual colonoscopy)
- Tests for blood in the stool
- Stool DNA tests
- Sigmoidoscopy
Your health care provider may have other reasons to recommend a colonoscopy.
What are the risks of a colonoscopy?
As with any invasive procedure, complications may occur. Complications related to colonoscopy include, but are not limited to, the following:
- Continued bleeding after biopsy (tissue sample) or polyp removal
- Nausea, vomiting, bloating or rectal irritation caused by the procedure or by the preparatory bowel cleansing
- A bad reaction to the pain medicine or the sedative (medicine used to provide a relaxing, calming effect)
- A perforation (hole) in the intestinal wall, which is a rare complication
You may have other risks related to your condition. Be sure to discuss any concerns with your provider before the procedure.
How do I get ready for a colonoscopy?
Your health care provider will fully explain the procedure and answer your questions. You will be asked to sign a consent form prior to the test. Read the form carefully and ask any questions you may have.
Dietary Instructions
You must not eat or drink for a specified amount of time before the procedure. This often means no food or drink after midnight or a restricted schedule with the laxative and water sips allowed until a couple hours before the colonoscopy. You may be given additional instructions about a special diet to follow for one or two days before the procedure. It is absolutely mandatory to follow your particular instructions carefully to avoid cancellation and to ensure a safe, effective test.
Notifications for Your Doctor
Before your colonoscopy, tell your provider:
- If you are sensitive or allergic to any medicines, latex, tape oranesthesia medicines (local and general)
- About all the medicines you take, including over-the-counter drugs, prescription medicines, vitamins, herbs and other supplements
- If you have a history of bleeding disorders
- If you are pregnant or think you may be pregnant
Bowel Preparation
Your health care provider will give you instructions on how to prepare your bowel for the test. You may be asked to take a laxative, an enema or a rectal laxative suppository. Or you may have to drink a special fluid that helps clean out your colon.
Medications Before and After the Procedure
If you are taking any blood-thinning medicines, aspirin, ibuprofen or other medicines that affect blood clotting, they may need to be stopped before the procedure. If you have a heart valve disease, you may be given disease-fighting antibiotics before the procedure.
Prior to the procedure, you will be given pain medicine and a sedative. After the procedure, someone must drive you home.
The Importance of Good Bowel Preparation During Colonoscopy
In this video, learn why the bowel preparation for a colonoscopy is so important to the results of the procedure.
What happens during a colonoscopy?
You may have a colonoscopy in an outpatient setting or as part of your stay in a hospital. The way the test is done may vary depending on your condition and your health care provider's practices.
Generally, the colonoscopy follows this process:
- You will be asked to remove any jewelry or other objects that mightget in the way during the procedure.
- You may be asked to remove your clothing and put on a hospital gown.
- An intravenous (IV) line will be inserted into your arm or hand. A sedative or a pain medicine will be injected into the IV.
- You will be given oxygen to breathe.
- Your heart rate, blood pressure, respiratory rate and oxygen level will be checked during the procedure.
- You will be asked to lie on your left side with your knees pulled up towards your chest.
- A lubricated tube will be put into your anus and moved into your rectum and colon. You may feel mild pain, pressure or cramping during the procedure. A sedative is used to reduce your discomfort.
- Depending on the type of anesthesia used, you may be completely asleep during the procedure. If awake, you may be asked to take slow, deep breaths while the tube is being inserted. This helps to relax your abdominal muscles and decrease the discomfort. You may also be asked to change your position to help the tube pass through.
- Air may be injected into your bowel. This may make it easier to see the inside surfaces. A water jet may also be used to clean the lining of your colon. A suction device may be used to remove any liquid stool.
- The health care provider will check your colon and may take photos. If a polyp is seen, it may be taken out. Or it may be left in the colon until a future procedure is performed.
- After the procedure is over, the tube will be taken out.

Need to learn more about colorectal cancer?
Our team is dedicated to developing multidisciplinary treatment plans for complicated, advanced colon and rectal cancers.
What happens after a colonoscopy?
After the procedure, you will be taken to the recovery room to be monitored. Your recovery process will depend on the type of sedative you were given. Once your blood pressure, pulse and breathing are stable and you are awake and alert, you will be taken to your hospital room. Or you may be discharged to your home.
You can usually eat whatever you can tolerate after the procedure. Some people start with small, bland meals.
It is normal to be flatulent (pass gas) and experience gas pains after the procedure. Walking and moving around may help to ease any mild pain.
You should not drink alcohol for at least 24 hours. You may be asked to drink extra fluids to make up for the water you lost as you got ready for the procedure.
Tell your provider if you experience any of the following:
- Fever or chills
- Frequent, bloody stools
- Belly pain or swelling
- A hardened belly
- The inability to pass gas
Your health care provider may give you other instructions depending on your situation.