Craniotomy
What is a craniotomy?
A craniotomy is the surgical removal of part of the bone from the skull to expose the brain. Specialized tools are used to remove the section of bone called the bone flap. The bone flap is temporarily removed, then replaced after the brain surgery has been done.
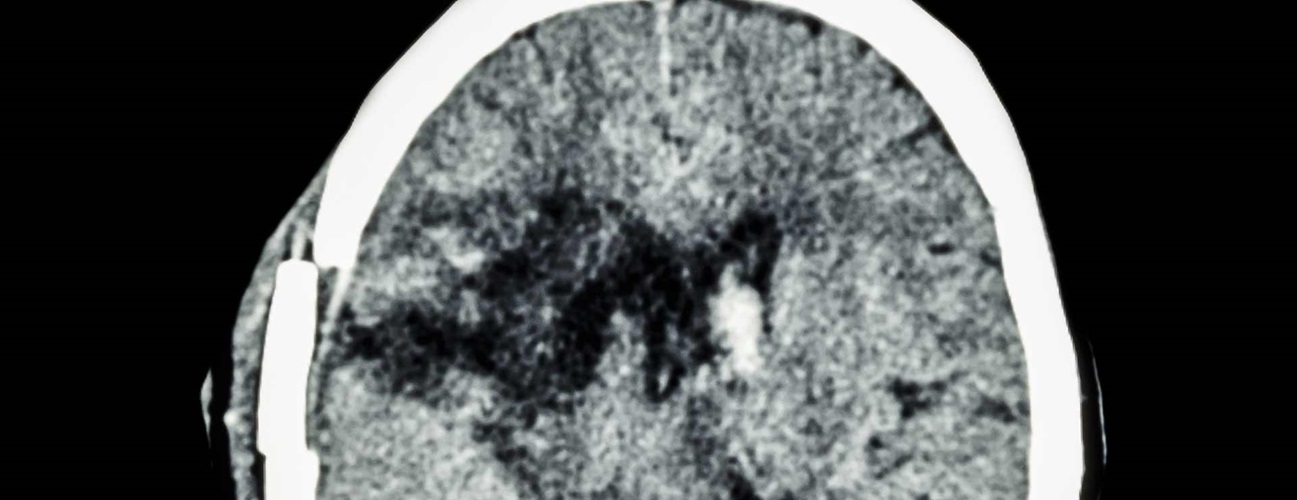
Some craniotomy procedures may use the guidance of computers and imaging (magnetic resonance imaging [MRI] or computerized tomography [CT] scans) to reach the precise location within the brain that is to be treated. This technique requires the use of a frame placed onto the skull or a frameless system using superficially placed markers or landmarks on the scalp. When either of these imaging procedures is used along with the craniotomy procedure, it is called stereotactic craniotomy.
Scans made of the brain, in conjunction with these computers and localizing frames, provide a three-dimensional image, for example, of a tumor within the brain. It is useful in making the distinction between tumor tissue and healthy tissue and reaching the precise location of the abnormal tissue.
Other uses include stereotactic biopsy of the brain (a needle is guided into an abnormal area so that a piece of tissue may be removed for exam under a microscope), stereotactic aspiration (removal of fluid from abscesses, hematomas, or cysts), and stereotactic radiosurgery (such as gamma knife radiosurgery).
An endoscopic craniotomy is another type of craniotomy that involves the insertion of a lighted scope with a camera into the brain through a small incision in the skull.
Aneurysm clipping is another surgical procedure which may require a craniotomy. A cerebral aneurysm (also called an intracranial aneurysm or brain aneurysm) is a bulging weakened area in the wall of an artery in the brain, resulting in an abnormal widening or ballooning. Because of the weakened area in the artery wall, there is a risk for rupture (bursting) of the aneurysm. Placement of a metal clip across the "neck" of the aneurysm isolates the aneurysm from the rest of the circulatory system by blocking blood flow, thereby preventing rupture.
Craniectomy is a similar procedure during which a portion of the skull is permanently removed or replaced later during a second surgery after the swelling has gone down. .
Other related procedures that may be used to diagnose brain disorders include cerebral arteriogram , computed tomography (CT) scan of the brain , electroencephalogram (EEG) , magnetic resonance imaging (MRI) of the brain , positron emission tomography (PET) scan , and X-rays of the skull . Please see these procedures for additional information.

Our Approach to Craniotomy
Johns Hopkins neurosurgeons are highly skilled and experienced in all types of craniotomy including newer, less invasive options for brain tumor surgery, aneurysm surgery and other procedures. In addition, a specialized clinic offers patients safe repair of skull deformities after brain surgery.
Types of Craniotomy
Extended Bifrontal Craniotomy
The extended bifrontal craniotomy is a traditional skull base approach used to target difficult tumors toward the front of the brain. It is based on the concept that it is safer to remove extra bone than to unnecessarily manipulate the brain.
The extended bifrontal craniotomy involves making an incision in the scalp behind the hairline and removing the bone that forms the contour of the orbits and the forehead. This bone is replaced at the end of surgery. Temporarily removing this bone allows surgeons to work in the space between and right behind the eyes without having to unnecessarily manipulate the brain.
The extended bifrontal craniotomy is typically used for those tumors that are not a candidate for removal by minimally invasive approaches because of either the anatomy of the tumor, the possible pathology of the tumor or the goals of surgery.
Types of tumors treated with the extended bifrontal craniotomy include meningiomas , esthesioneuroblastomas and malignant skull base tumors .
Minimally Invasive Supra-Orbital “Eyebrow” Craniotomy
Supra-orbital craniotomy (often called "eyebrow" craniotomy) is a procedure used to remove brain tumors. In this procedure, neurosurgeons make a small incision within the eyebrow to access tumors in the front of the brain or around the pituitary gland, which is deeper in the brain behind the nose and eyes. This approach is used instead of endonasal endoscopic surgery when a tumor is very large or close to the optic nerves or vital arteries.
Because it is a minimally invasive procedure, supra-orbital “eyebrow” craniotomy may offer
-
Less pain than open craniotomy
-
Faster recovery than open craniotomy
-
Minimal scarring
The supra-orbital craniotomy may be part of the treatment for Rathke’s cleft cysts, skull base tumors and some pituitary tumors.
Retro-Sigmoid “Keyhole” Craniotomy
Retro-sigmoid craniotomy (often called "keyhole" craniotomy) is a minimally-invasive surgical procedure performed to remove brain tumors. This procedure allows for the removal of skull base tumors through a small incision behind the ear, providing access to the cerebellum and brainstem. Neurosurgeons may use this approach to reach certain tumors, such as meningiomas, acoustic neuromas (vestibular schwannomas), skull base tumors and metastatic brain tumors.
Benefits of "keyhole" craniotomy includes less pain after the procedure than after an open craniotomy, less scarring and a more rapid recovery.
Orbitozygomatic Craniotomy
The orbitozygomatic craniotomy is a traditional skull base approach used to target difficult tumors and aneurysms. It is based on the concept that it is safer to remove extra bone than to unnecessarily manipulate the brain.
Typically used for those lesions that are too complex for removal by more minimally invasive approaches, orbitozygomatic craniotomy involves making an incision in the scalp behind the hairline and removing the bone that forms the contour of the orbit and cheek. This bone is replaced at the end of surgery. Temporarily removing this bone allows surgeons to reach deeper and difficult parts of the brain while minimizing severe damage to the brain.
Brain tumors that may be treated with orbitozygomatic craniotomy include craniopharyngiomas, pituitary tumors and meningiomas.
Translabyrinthine Craniotomy
A translabyrinthine craniotomy is a procedure that involves making an incision in the scalp behind the ear, then removing the mastoid bone and some of the inner ear bone (specifically, the semicircular canals which contain receptors for balance). The surgeon then finds and removes the tumor, or as much of the tumor as possible without risk of severe damage to the brain.
When there is no useful hearing or hearing is to be sacrificed, the translabyrinthine approach is often considered for removal of acoustic neuromas. During the translabyrinthine craniotomy, the semicircular canals of the ear are removed in order to access the tumor. Complete hearing loss occurs as a result of the removal of the semicircular canals.
Although hearing is lost with the translabyrinthine craniotomy, the risk of facial nerve injury may be reduced.
Reasons for the procedure
A craniotomy may be done for a variety of reasons, including, but not limited to, the following:
-
Diagnosing, removing, or treating brain tumors
-
Clipping or repairing of an aneurysm
-
Removing blood or blood clots from a leaking blood vessel
-
Removing an arteriovenous malformation (AVM) or addressing an arteriovenous fistula (AVF)
-
Draining a brain abscess, which is an infected pus-filled pocket
-
Repairing skull fractures
-
Repairing a tear in the membrane lining the brain (dura mater)
-
Relieving pressure within the brain (intracranial pressure) by removing damaged or swollen areas of the brain that may be caused by traumatic injury or stroke
-
Treating epilepsy
-
Implanting stimulator devices to treat movement disorders such as Parkinson's disease or dystonia (a type of movement disorder)
There may be other reasons for your doctor to recommend a craniotomy.
Risks of the procedure
As with any surgical procedure, complications may occur. Brain surgery risk is tied to the specific location in the brain that the operation will affect. For example, if the area of the brain that controls speech is operated on, then speech may be affected. Some more general complications include, but are not limited to, the following:
-
Infection
-
Bleeding
-
Blood clots
-
Pneumonia (infection of the lungs)
-
Unstable blood pressure
-
Seizures
-
Muscle weakness
-
Brain swelling
-
Leakage of cerebrospinal fluid (the fluid that surrounds and cushions the brain)
-
Risks associated with the use of general anesthesia
The following complications are rare and generally relate to specific locations within the brain, so they may or may not be valid risks for certain individuals:
-
Memory problems
-
Speech difficulty
-
Paralysis
-
Abnormal balance or coordination
-
Coma
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Before the procedure
-
Your doctor will explain the procedure to you and you can ask questions.
-
You will be asked to sign a consent form that gives permission to do the surgery. Read the form carefully and ask questions if something is not clear.
-
In addition to a complete medical history, your doctor will do a physical exam to ensure you are in good health before you undergo the surgery. You may also need blood tests and other diagnostic tests.
-
You will receive a preoperative neurological exam that will be used to compare with postoperative exams.
-
You will be asked to fast before the procedure, generally after midnight.
-
If you are pregnant or think you may be, tell your healthcare provider.
-
Tell your doctor if you are sensitive to or are allergic to any medicines, latex, tape and anesthetic agents (local or general).
-
Tell your doctor of all medicines (prescribed and over-the-counter) and herbal supplements that you are taking.
-
Tell your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect blood clotting. It may be necessary for you to stop these medicines before the procedure.
-
If you smoke, you should stop smoking as soon as possible before the procedure to improve your chances for a successful recovery from surgery and to improve your overall health status.
-
You may be asked to wash your hair with a special antiseptic shampoo the night before the surgery.
-
You may receive a sedative before the procedure to help you relax.
-
The areas around the surgical site will be shaved.
-
Based on your medical condition, your doctor may request other specific preparation.
.ashx?h=200&iar=0&mh=360&mw=520&w=200&hash=D6A61835B7EE818C60BC555D169157E4)
During the procedure
A craniotomy generally requires a hospital stay of 3 to 7 days. You may also go to a rehabilitation unit for several days after your hospital stay. Procedures may vary depending on your condition and your doctor's practices.
Generally, a craniotomy follows this process:
-
You will be asked to remove any clothing, jewelry, or other objects that may interfere with the procedure.
-
You will be given a gown to wear.
-
An intravenous (IV) line will be inserted in your arm or hand.
-
A urinary catheter will be inserted to drain your urine.
-
You will be positioned on the operating table in a manner that provides the best access to the side of the brain to be operated on.
-
The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
-
Your head will be shaved and the skin over the surgical site will be cleansed with an antiseptic solution.
-
There are various types of incisions that may be used, depending on the affected area of the brain. An incision may be made from behind the hairline in front of your ear and the nape of your neck, or in another location depending on the location of the problem. If an endoscope is used, the incisions may be smaller.
-
Your head will be held in place by a device which will be removed at the end of the surgery.
-
The scalp will be pulled up and clipped to control bleeding while providing access to the brain.
-
A medical drill may be used to make burr holes in the skull. A special saw may be used to carefully cut the bone.
-
The bone flap will be removed and saved.
-
The dura mater (the thick outer covering of the brain directly underneath the bone) will be separated from the bone and carefully cut open to expose the brain.
-
Excess fluid will be allowed to flow out of the brain, if needed. Microsurgical instruments, such as a surgical microscope to magnify the area being treated, may be used. This can enable the surgeon a better view of the brain structures and distinguish between abnormal tissue and healthy tissue. Tissue samples may be sent to the lab for testing.
-
A device, such as a drain or a special type of monitor, may be placed in the brain tissue to measure the pressure inside the skull, or intracranial pressure (ICP). ICP is pressure created by the brain tissue, cerebral spinal fluid (CSF), and blood supply inside the closed skull.
-
Once the surgery is completed, the surgeon will suture (sew) the layers of tissue together.
-
The bone flap will be reattached using plates, sutures, or wires.
-
If a tumor or an infection is found in the bone, the flap may not be replaced. Also, if decompression (to reduce pressure in the brain) is required, the bone flap may not be replaced.
-
The skin incision (scalp) will be closed with sutures or surgical staples.
-
A sterile bandage or dressing will be applied over the incision.

What to Expect After Brain Surgery | Webinar
Successful surgery to the brain or skull requires a skilled neurosurgeon. And knowing what to expect after this type of procedure can help ensure a successful recovery. In this presentation neurosurgeon Raj Mukherjee discusses recovery in the hospital and at home, typical rehabilitation needs and what getting “back to normal” might look like.
After the procedure
In the hospital
Immediately after the procedure, you will be taken to a recovery room for observation before being taken to the intensive care unit (ICU) to be closely monitored. Or, you may be taken directly to the ICU from the operating room.
In the ICU, you may be given medicine to decrease the brain swelling.
Your recovery process will vary depending upon the type of procedure done and the type of anesthesia given. Once your blood pressure, pulse, and breathing are stable and you are alert, you may be taken to the ICU or your hospital room.
After staying in the ICU, you will move to a room on a neurosurgical nursing unit in the hospital. You will remain in the hospital for several more days.
You may need oxygen for a period of time after surgery. Generally, the oxygen will be discontinued before you go home.
You will be taught deep-breathing exercises to help re-expand the lungs and prevent pneumonia.
Frequent neurological checks will be done by the nursing and medical staff to test your brain function and to make sure your body systems are functioning properly after your surgery. You will be asked to follow a variety of basic commands, such as moving your arms and legs, to assess your brain function. Your pupils will be checked with a flash light, and you will be asked questions to assess your orientation (such as your name, the date, and where you are). The strength of your arms and legs will also be tested.
The head of your bed may be elevated to prevent swelling of your face and head. Some swelling is normal.
You will be encouraged to move around as tolerated while in bed and to get out of bed and walk around, with assistance at first, as your strength improves. A physical therapist (PT) may be asked to evaluate your strength, balance, and mobility, and give you suggestions for exercises to do both in the hospital and at home.
You will likely have sequential compression devices (SCDs) placed on your legs while you are in bed to prevent blood clot formation. SCDs have an air compressor that slowly pumps air into and out of fitted sleeves that are placed on the legs. They help prevent blood clots from forming by passively compressing the leg veins to keep blood moving.
Depending on your situation, you may be given liquids to drink a few hours after surgery. Your diet may be gradually changed to include more solid foods as you can handle them.
You may have a catheter in your bladder to drain your urine for a day or so, or until you are able to get out of bed and move around. Be sure to report any painful urination or other urinary symptoms that occur after the catheter is removed, as these may be signs of an infection that can be treated.
Depending on your status, you may be transferred to a rehabilitation facility for a period of time to regain your strength.
Before you are discharged from the hospital, arrangements will be made for a follow-up visit with your doctor. Your doctor will also give you instructions for home care.
At home
Once you are home, it is important to keep the incision clean and dry. Your doctor will give you specific bathing instructions. If stitches or surgical staples are used, they will be removed during a follow-up office visit. If adhesive strips are used, keep them dry and they will fall off within a few days.
You may choose to wear a loose turban or hat over the incision. You should not wear a wig until the incision is completely healed (about 3 to 4 weeks after surgery).
The incision and head may ache, especially with deep breathing, coughing, and exertion. Take a pain reliever for soreness as recommended by your doctor. Aspirin or other blood thinning medicines may increase the chance of bleeding. Be sure to take only recommended medicines and ask if you are unsure.
Continue the breathing exercises used in the hospital to prevent lung infection. You will be advised to avoid exposure to upper respiratory infections (colds and flu) and irritants, such as tobacco smoke, fumes, and environmental pollution.
You should gradually increase your physical activity as you can handle them. It may take several weeks to return to your previous level of energy and strength.
You may be instructed to avoid lifting heavy items for several weeks to prevent strain on your surgical incision.
Do not drive until your doctor gives you permission.
Call your doctor to report any of the following:
-
Fever or chills
-
Redness, swelling, drainage, or bleeding or other drainage from the incision site or face
-
Increased pain around the incision site
-
Vision changes
-
Confusion or excessive sleepiness
-
Weakness of your arms or legs
-
Trouble with speech
-
Trouble breathing, chest pain, anxiety, or change in mental status
-
Green, yellow, or blood-tinged sputum (phlegm)
-
Seizure activity
Following a craniotomy, your doctor may give you other instructions, depending on your particular situation.