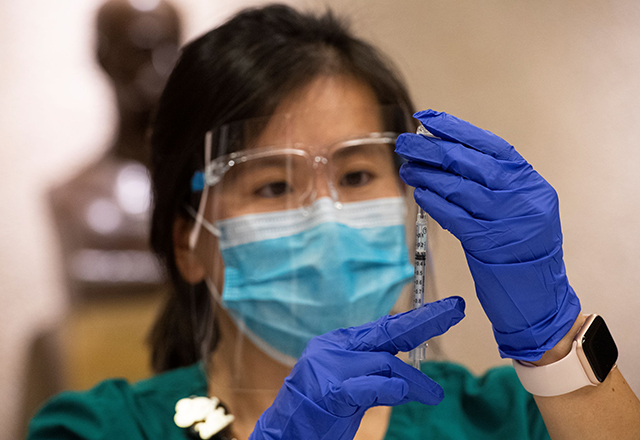
‘This will hopefully end the pandemic.’ — Denise Fu
On the morning of Dec. 16, Denise Fu was tapped to draw up and prepare the first set of COVID-19 vaccinations to be administered to front-line faculty and staff members at The Johns Hopkins Hospital. It wasn’t a particularly complicated task, but she admits that the historic nature of the moment made her a wee bit nervous.
“The Pfizer vaccine needs to be diluted and then drawn up, which takes more time, so that was a role Pharmacy could play well,” says Fu, clinical programs manager for outpatient pharmacy services for the Johns Hopkins Home Care Group. Fu and her three team members are state-certified vaccinators, which allows them to inject the vaccine into the arms of recipients in addition to drawing up the vaccine syringes.
“My primary role right now is finding pharmacists to participate in the COVID-19 vaccination program, and I help fill in holes when we don’t have others available,” says Fu. “I have about 100 pharmacist volunteers (from The Johns Hopkins Hospital and Home Care Group) certified to vaccinate who I’m coordinating with Occupational Health. I am also working on training pharmacy students as well.”
Fu, who lives in the Canton neighborhood in Baltimore City and joined Johns Hopkins in 2011, says she’s excited to participate in the COVID-19 vaccination program. “This will hopefully end the pandemic,” she says.
Among her regular duties, Fu supervises a team of clinical pharmacists for medication therapy and works with pharmacy managers at 10 outpatient pharmacy locations to standardize clinical initiatives.
COVID-19 has dramatically changed the in-home visitation and in-pharmacy education aspects of the work performed by Fu and her Home Care Pharmacy colleagues. Often, during a hospital stay, a patient’s medications may be altered in significant ways, through additions, deletions and changes in doses that must be adhered to for safety and efficacy. Prior to the pandemic, Fu and her colleagues would often visit patients in their homes to help manage medications.
“We stopped doing the home visits and switched to telephoning the patients to follow up with them,” says Fu. “We also stopped having patients come into the pharmacies for appointments because our consult rooms are very tiny rooms where you can’t really have physical distance. Now, we hand-deliver medication pillboxes to the patient at the door, and then we follow up with a phone call asking how they are doing, are they remembering to take their meds and how can we continue to support them. A lot has changed.”
Posted Jan. 25, 2021
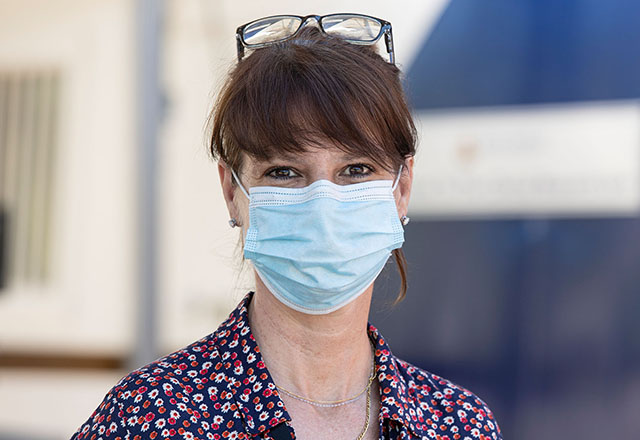
“Some people are eager to help, and some are afraid. I try to be there and just listen. My heart goes out to people. ” — Catherine Wren
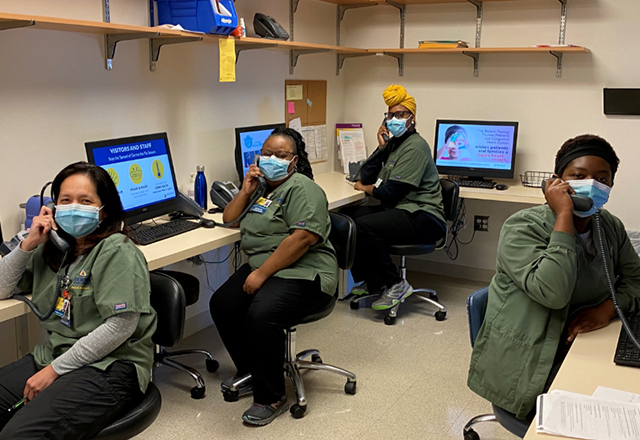
For the past 15 years, Catherine Wren has worked on Johns Hopkins clinical research studies at locations of community mental health programs across Maryland. Since April, however, the research coordinator has reported to work at a remote parking lot at Green Spring Station that features two mobile trailers, two mobile offices with negative air pressure and a large tented area connecting them.
“We were all pulled from different jobs and different areas to work on the COVID studies. It happened lickety-split,” Wren says.
At the field-based clinical research site, Wren collects vital signs, draws blood and performs COVID-19 testing. “This is new for all of us,” says Wren, noting that the research participants bring different emotions and motivations. “Some people are eager to help, and some are afraid. I try to be there and just listen. My heart goes out to people.”
To learn about participating in these and other studies, visit COVID-19 Research Opportunities for Employees, or join the Johns Hopkins COVID-19 Study Interest Outreach Registry.
Read more about Catherine Wren's career at Johns Hopkins.
Posted Aug. 21, 2020
“I enjoy helping people when I can. That’s what motivates me.” — Rickey Jenkins
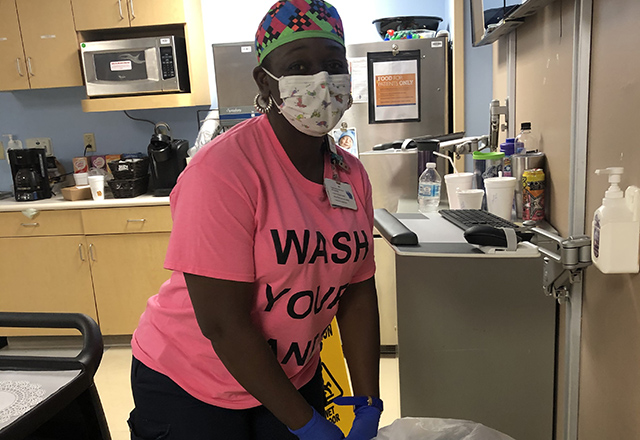
Johns Hopkins hospitals have adopted a range of new procedures and safeguards to help protect patients and staff from COVID-19, and keeping the environment clean and safe from hazards has never been more important.
Rickey Jenkins has taken the new protocols to heart. He joined the Environmental Services team at Howard County General Hospital as a floor technician in 2015. In addition to disinfecting areas on their routine rounds, Jenkins and his colleagues listen for the “Bat Phone,” which rings whenever urgent cleaning services are needed.
The Bat Phone often sends him to the emergency department (ED), where he notes the teamwork and professionalism of the nurses and doctors. He says, “The ED is amazing. They’re on it; they do their job. Whatever is going on with them, they stay focused on caring for the patient.”
Likewise, he says, “I enjoy helping people when I can. That’s what motivates me.”
Being on the front lines during the pandemic isn’t easy, but Jenkins knows he’s not facing the challenge alone. His family is supportive, and so are his colleagues.
“We have proper personal protective equipment so we can do a good job and keep people safe. We work together well, because that’s what the job requires.”
Posted Aug. 14, 2020
“Before you enter a room, it takes a few minutes to mentally review everything you’re supposed to have on.” — Ladonna Bingham
As interim chief of critical care and interim medical director of the pediatric intensive care unit at Johns Hopkins All Children’s Hospital (JHACH) in Florida, Ladonna Bingham ensures that people comply with safety precautions. Lately, Bingham — a 15-year JHACH veteran — has spent extra hours in meetings to review protocols and update policies for patients diagnosed with COVID-19. Every day brings six to eight new patients from the emergency room who may have the disease.
“Before you enter a room, it takes a few minutes to mentally review everything you’re supposed to have on,” she says. “Being extra careful with the donning and doffing, and getting respiratory therapies performed safely, adds another layer of complexity to the care. I’m so impressed to see how people on our team and across the system have rallied together to adapt.”
Posted Aug. 12, 2020
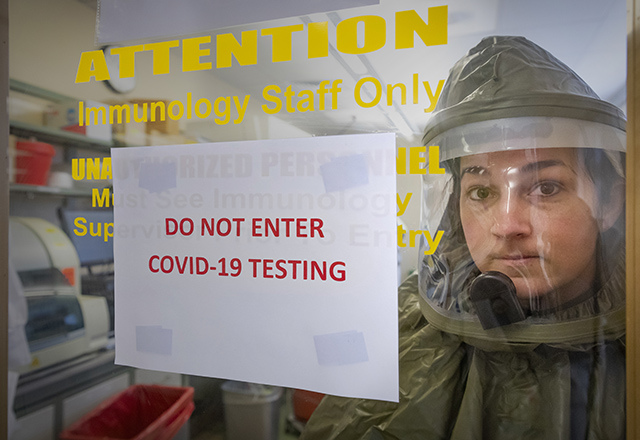
“Knowing that I’m making a difference is gratifying.” — Bethany Peters
Bethany Peters is the lead medical technologist in the Clinical Molecular Genetics Lab at Johns Hopkins All Children’s Hospital, so she is accustomed to handling samples with care. But helping the hospital’s immunology team perform COVID-19 testing requires a new level of vigilance. “I joke that I’m putting on a space suit,” she says. “The way you handle and process samples is more meticulous and cautious.” Peters credits Sarah Dodge and her immunology lab team with developing the test Johns Hopkins All Children’s runs. “We do not just open a box and throw it on a machine. The entire process is far more extensive.”
Peters says it’s important to remember that many medical laboratory professionals work behind the scenes, making discoveries and taking risks. Amid a pandemic, she’s happy to do her part: “Knowing that I’m making a difference is gratifying. I think all of us who work in the hospital setting generally feel this way. But right now, this feeling is taken to a whole other level.”
Posted July 28, 2020
 Click to enlarge. Photo credit: Keith Weller
Click to enlarge. Photo credit: Keith Weller“It’s been very exciting to see so many COVID-19 survivors step up to donate their antibody-rich blood to save other lives.” — Shmuel Shoham, M.D.
Shmuel Shoham, M.D., has spent most of his nine years at Johns Hopkins diagnosing and caring for patients with infectious diseases, such as pneumonia. But when COVID-19 cases began to soar — with no cure in sight — the associate professor of medicine in the transplant and oncology infectious diseases program felt compelled to act. Building on previous research to treat influenza using antibodies from survivors’ blood, Shoham helped form a consortium of experts to launch clinical trials investigating COVID-19 survivor blood as a treatment.
“Suddenly I was putting in 18-hour days,” he says. Results from these initial studies proved promising, but there weren’t enough blood donors for those who needed it. Knowing that New York’s Orthodox Jewish community was hard hit with COVID-19, Shoham called a friend there for help. Within five weeks, enough plasma was collected to treat more than 7,000 hospitalized COVID-19 patients throughout the country.
Shoham and his colleagues are part of the 57-institution National COVID-19 Convalescent Plasma Project to oversee, research and publicize this treatment. “It’s been very exciting to see so many COVID-19 survivors step up to donate their antibody-rich blood to save other lives,” says Shoham.
Posted July 22, 2020
“I feel I need to be here for my staff, our providers and our patients.” — Teira Torbit
Teira Torbit is a practice administrator for Johns Hopkins Community Physicians in Howard County. She leads a team of 15 people who work together to keep the family medicine practice running.
These days, that involves screening patients for COVID-19. “We have plenty of protective equipment,” she says. “It’s helpful to have the support I need to do my job.”
Teira has also worked to get the practice’s telemedicine program up to speed on short notice. “One minute we were doing our regular job, and the next, we switched to telemedicine. We had to ramp up pretty fast.”
“I love caring for patients, and I love my staff,” the Baltimore native says. “I make sure staff and providers understand how much we appreciate everything they’re doing.”
Posted June 10, 2020
“My colleagues and I are ready to do what it takes to help our patients and society.” — Nisar Yaseen
A family medicine specialist with a clinical interest in chronic pain, Nisar Yaseen has worked at Johns Hopkins Aramco Healthcare (JHAH) since 2017. He also serves as a senior trainer within the JHAH family medicine residency program.
Yaseen says COVID-19 has had a “huge impact” on his job due to the sudden change from seeing patients in regular clinics to using telemedicine and unfamiliar work environments to manage primary and urgent care.
“The best thing about work right now is the pleasure of collaborating with various clinical and nonclinical colleagues in an amazing, versatile and resilient multidisciplinary team,” he says.
“Not really knowing how this situation will pan out in the short term is challenging, but it is offset by knowing that whatever happens, my colleagues and I are ready to do what it takes to help our patients and society.”
Posted June 8, 2020
“The best part about my redeployment has been getting to know the dietary staff and seeing patients in a different way.” — Rob Grader
Normally, Howard County General Hospital physical therapist assistant Rob Grader spends his days guiding patients through rehabilitation post-joint replacement or for a medical condition. But since the pandemic began, demand for PT services has waned, so he was redeployed to help out in food services. Now, every work day, from 6 a.m. to 2:30 p.m., Grader gowns up and delivers meals to patients throughout the hospital.
“It’s been an adjustment,” says Grader, “but I imagine these patients are bored and isolated, and I appreciate the brief opportunity to interact with them.” (He’s not permitted to enter COVID-19 unit rooms.) As he sets the meal down on the table, he might ask patients what they’re reading “just to have a momentary interaction — what I enjoy about my other job, too.”
Grader has new respect for the dietary team — “a pretty great bunch of people, working nonstop.” Pandemic or not, he points out, everyone needs to eat. “Obviously, I’m eager to get back to the work I’m trained for and enjoy,” says Grader, “but this is an all-hands-on-deck situation, and I’m happy to do something helpful.”
Posted June 3, 2020
“Although we are a small piece of what goes on in the hospital, we are a very important piece.” — Annette Jenkins
Annette Jenkins, a 31-year employee of Johns Hopkins All Children’s Hospital, is a supply chain supervisor who is “extremely proud to be on the front line” of the response to COVID-19. Here she’s selecting personal protective equipment (gloves) for a nurse. Because of the pandemic, she now receives large deliveries of COVID-19 related items that ensure physicians have everything they may require.
Married to Willie Jenkins, recently retired All Children’s food service cook, Jenkins reminds her staff members “to perform their duties as if it were their child or grandchild being cared for. Although we are a small piece of what goes on in the hospital, we are a very important piece.”
Posted June 1, 2020
“It’s up to us to make sure those rooms are absolutely free of that virus.” — Roark Nixon
As environmental services manager at Howard County General Hospital, Roark Nixon leads a team responsible for cleaning and disinfecting rooms after patients are moved or discharged. Since March, that has included eliminating any new coronavirus present in hospital rooms.
"When a patient leaves, we bring in an ultraviolet light that kills the virus,” he says. "Then we scrub the whole thing down from top to bottom with a bleach-based disinfectant. And after that, we bring the light back in and clean the room again."
The work requires training and concentration. Nixon says the environmental services staff is “holding up pretty well during all this. They’ve really adapted to new workflows and protocols.”
In this photograph, Nixon is readying disinfectant canisters for distribution throughout the hospital. “Each one holds a disinfectant used for a different purpose,” he explains. “The orange one is the one with the bleach in it.”
Posted May 28, 2020
“I hope that the food I prepare can bring some sort of comfort." — Miriam Zepeda
A cook in Howard County General Hospital’s Food and Nutrition Services for 12 years, Miriam Zepeda says that while she takes “great pleasure” in her work, the pandemic has brought a few extra challenges.
“The temperatures in the kitchen are already hot, and the face mask makes it difficult to breathe. There is also an influx of patients, and I try my best to make sure food is prepared in a timely manner.
“Even though we may not be working on the front lines with patients, we are still working very hard to provide the best service,” says the resident of Columbia, Maryland. “I hope that the food I prepare can bring some sort of comfort to someone who may not be feeling their best.”
Posted May 26, 2020
“It’s gratifying to be able to care for people, especially during these nerve-racking times.” — Daliah Halboni
Daliah Halboni says she always wanted to be a nurse. For the last two years, the critical care specialist has answered that calling at Johns Hopkins Community Physicians in Howard County. During the pandemic, she says it is especially important to find the best way to serve each patient. While many will use the office’s telemedicine option, others need to go to the office for services ranging from electrocardiograms to ear exams. Halboni also uses her clinical knowledge to recommend when callers should go to the emergency department. So far, at least one patient has thanked Halboni for saving her life.
Halboni screens patients and helps ensure the examination rooms are clean, disinfected and stocked with gowns and other supplies. “It’s gratifying to be able to care for people, especially during these nerve-racking times,” she says. “It means so much to hear the voices of patients on the phone saying they’re glad we're open.”
Posted May 21, 2020
“I am proud to be a nurse leader.” — Chrystal Brown
At Sibley Memorial Hospital and other Johns Hopkins hospitals, care providers are finding new ways to treat patients. Chrystal Brown, primary care practice manager, has been working at Sibley’s drive-through testing area.
“I am proud to be a nurse leader,” says Chrystal Brown, primary care practice manager. “I work for such a wonderful organization and with people who want to do their part by performing COVID-19 testing. Prior to this assignment, I was managing the offices of primary care and specialty services. Now, I split my time between the testing tent and primary care. Presently, roughly 90% of our appointments are video visits.”
Posted May 18, 2020
“Wearing my ‘Happy Birthday’ crown that day seemed to give everyone a lift.” — Dawn Silver
Dawn Silver, a food services hostess at Johns Hopkins Bayview Medical Center, knew people would notice when she arrived at work wearing a crown. “It was my birthday, and I had to work,” she says, “so why not wear a crown? Wearing my happy birthday crown that day seemed to give everyone a lift.
Pandemic precautions prohibit food services staff members from working on COVID-19 units. The 16-year dietary services veteran says she misses the camaraderie that delivering trays to patients brings. “But we have to be extra careful now, washing our hands constantly and making sure we don’t have symptoms,” says Silver. “I want people to know that food services workers have an important role working on the front lines of this pandemic."
Posted May 15, 2020
“We’re making sure patients get the care they need and deserve — whatever it takes.” — Lynne Lightfoote
Sibley Memorial Hospital obstetrician and gynecologist Lynne Lightfoote has found that COVID-19 makes it challenging to maintain the compassionate relationships she usually has with her obstetrical patients. Although protective, the masks and additional personal protective equipment pose a barrier to the nonverbal communication that typically engenders trust. However, Lightfoote, who lives in Arlington, Virginia, says the pandemic has increased camaraderie among physicians and nurses as they strive to support each other. “We all work better together,” she says. “Our team of doctors and nurses are making sure patients get the care they need and deserve — whatever it takes.”
Posted May 14, 2020
Honoring All Our Health Care Professionals This Week
On May 10, many health care organizations across the country began observing National Hospital Week. We want to ensure that all our health care professionals are recognized for their contributions, so today, join us in celebrating Health Care Week at Johns Hopkins Medicine.
Posted May 11, 2020
Community Appreciation Parade for Healthcare Heroes
The Community Appreciation Parade for #HopkinsHeroes on May 7 was a gigantic boost of energy — more than 40 cars long — for all our front-line staff members. Our #HealthcareHeroes have been working tirelessly, with amazing strength, compassion and expertise, to treat all our patients during the COVID-19 pandemic. The toots, woo-woos, way-to-go’s, love and heartfelt thanks give us some of the fuel we need to keep going. Thank you!
Posted May 8, 2020
Nurses: Leading in the Midst of Crisis
Cynda Rushton is a professor at the Johns Hopkins School of Nursing and Berman Institute of Bioethics and an international leader in nursing ethics. On Global Promise, Johns Hopkins Medicine International’s blog, she discusses the conditions and decisions nurses encounter every day while wrestling with the massive health care challenges posed by the new coronavirus.
Go to the Global Promise blog.
Posted May 8, 2020
It’s Nurses Week: Thank You to All Our Nurses!
When it comes to patient care, our nurses have the strength to do the incredible. During Nurses Week, join us in recognizing our nursing colleagues across Johns Hopkins Medicine for the vital role they play every day.
Posted May 6, 2020
 Click to enlarge. Image courtesy: Marijoy Velasco, Apr. 22, 2020
Click to enlarge. Image courtesy: Marijoy Velasco, Apr. 22, 2020Behind the Scenes at the Johns Hopkins Outpatient Center Dermatology Department
Certified medical assistants for the Department of Dermatology at the Johns Hopkins Outpatient Center are in constant communication with colleagues to share ideas for providing the best patient care and service during the COVID-19 pandemic.
Posted May 4, 2020
 Click to enlarge. Image courtesy: Loraine Imwold.
Click to enlarge. Image courtesy: Loraine Imwold.U.S. Air Force Thunderbirds and Navy Blue Angels in Baltimore Flyover Salute to Healthcare Heroes
U.S. Air Force Thunderbirds and Navy Blue Angels honored our Healthcare Heroes today with an #AmericaStrong flyover in Baltimore to thank front-line staff members for responding in unprecedented ways to the COVID-19 pandemic.
We are so proud of all our #HopkinsHeroes for their compassion, courage and commitment to our patients — and to each other! Watch the flyover video here.
See more #HealthcareHeroesDay images on Johns Hopkins Medicine’s Facebook, Twitter and Instagram.
Posted May 2, 2020
 Click to enlarge. Image courtesy: Will Kirk
Click to enlarge. Image courtesy: Will KirkBlue Skies for Flyover Salute to Healthcare Heroes
Blue skies on a sunny day in Baltimore for the U.S. Air Force Thunderbirds and Navy Blue Angels as they honored #HealthcareHeroes with an #AmericaStrong flyover salute formation featuring six F-18 Hornet and six F-16 Fighting Falcon aircrafts. So proud of all our #HopkinsHeroes!
See more #HealthcareHeroesDay images on Johns Hopkins Medicine’s Facebook, Twitter and Instagram.
Posted May 2, 2020
 Visit the Johns Hopkins Medicine Facebook page for more images. Images courtesy: Will Kirk
Visit the Johns Hopkins Medicine Facebook page for more images. Images courtesy: Will KirkCheers and Awe for Flyover Salute to Healthcare Heroes
Johns Hopkins healthcare workers and their families were out in force to wave, cheer and salute the U.S. Air Force Thunderbirds and Navy Blue Angels during their #AmericaStrong flyover of hospitals honoring #HealthcareHeroes fighting the COVID-19 pandemic.
A formation of six F-16 Fighting Falcon and six F-18 Hornet aircrafts buzzed by Baltimore to say “thank you” for the compassion, courage and commitment of all front-line staff and first responders.
See more #HealthcareHeroesDay images on Johns Hopkins Medicine’s Facebook, Twitter and Instagram.
Posted May 2, 2020
Maryland Healthcare Heroes Day: We Stand With You
Governor Larry Hogan proclaimed May 2, 2020, as Heathcare Heroes Day in Maryland.
At Johns Hopkins Medicine, we stand with all of our healthcare workers, doctors, nurses, first responders and essential workers that have helped save lives and keep our state safe.
See more #HealthcareHeroesDay images on Johns Hopkins Medicine’s Facebook, Twitter and Instagram.
Posted May 2, 2020
“I chose medicine to have a positive impact and to help where needed.” — Monty Oppenheim
Monty Oppenheim, chief of obstetric anesthesiology at Sibley Memorial Hospital, where he’s practiced for 23 years, takes a rare moment on a busy day to enjoy the spring sun.
With operating rooms empty and elective surgeries postponed, Oppenheim has been reassigned. The father of four is now training as an intensivist to work on the front line of the new coronavirus pandemic. He will intubate patients with COVID-19, risking infection with every procedure.
He says, “This is my job. My colleagues and I chose medicine to have a positive impact and to help where needed. None of us expected this. COVID-19 is new to the medical world. We're still learning, striving to help our community survive this pandemic.”
Posted May 1, 2020
 Click to enlarge. Image courtesy: Sophie Lanzkron, Image taken: Apr. 11, 2020
Click to enlarge. Image courtesy: Sophie Lanzkron, Image taken: Apr. 11, 2020Marking 6-Feet-Apart Areas for Safe Physical Distancing at The Johns Hopkins Hospital
Sophie Lanzkron, M.D., director of the Sickle Cell Center for Adults at The Johns Hopkins Hospital snapped this photo, writing, “I have an incredible team of nurses, patient service coordinators and advanced practice providers who are taking care of our at-risk adults with sickle cell disease.
“They do everything from taking care of our patients, many of whom felt isolated before the pandemic, to taping off the floors to mark 6 feet distances to keep everyone safe. They have stepped up in every way, and I am really proud to be a part of their team!”
Posted Apr. 30, 2020
 Click to enlarge. Image taken: Apr. 8, 2020
Click to enlarge. Image taken: Apr. 8, 2020Johns Hopkins Community Physicians’ Offices in Action
Nurse Daliah Halboni (standing) and certified medical assistants Melody Kearny (center) and Jenna Seiss (right) help patients get the care they need during the coronavirus pandemic. At Johns Hopkins Community Physicians, care teams practice physical distancing and wear proper personal protective equipment, such as masks, to ensure the safety of both patients and staff members.
Posted Apr. 28, 2020
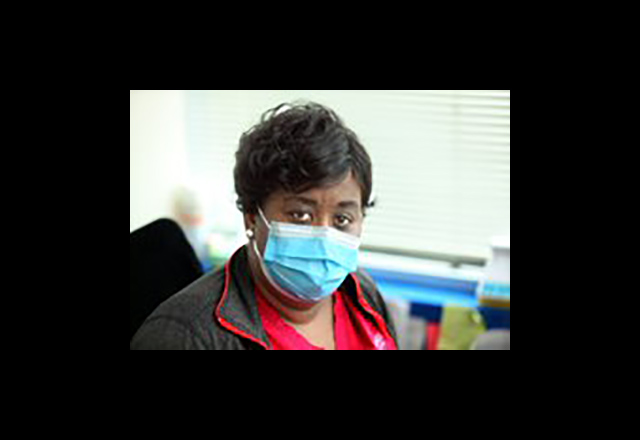
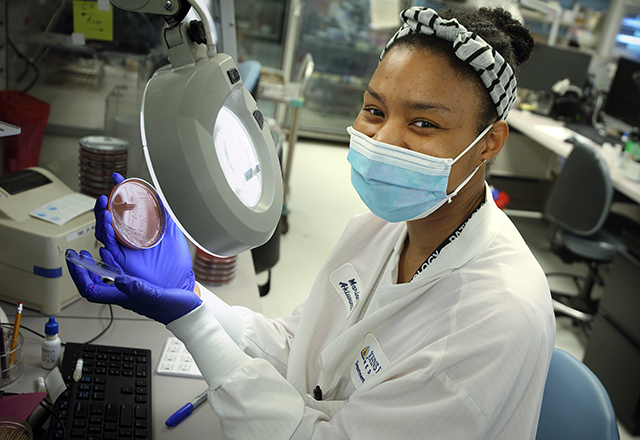
“We’re the hidden heroes.” — Marian Akiwumi
The most rewarding part of responding to the COVID-19 pandemic, says Marian Akiwumi, medical lab scientist in microbiology at The Johns Hopkins Hospital , is the teamwork. “We’ve grown better and more efficient,” says Akiwumi, a resident of Laurel who has worked at the hospital for three years. “As the microbiology department, we’re all doing our part by validating and running tests, producing COVID-19 results at great turnaround times. This is something that will go down in the history books.”
Akiwumi praises the work of everyone on the laboratory team. “We’re the hidden heroes,” she says. “We’re the ones that test everything so doctors and nurses know what’s happening with the patient. Without us, nothing is proved.”
Posted Apr. 25, 2020
 Click to enlarge. Image courtesy: Danielle Hirsch, Apr. 15, 2020
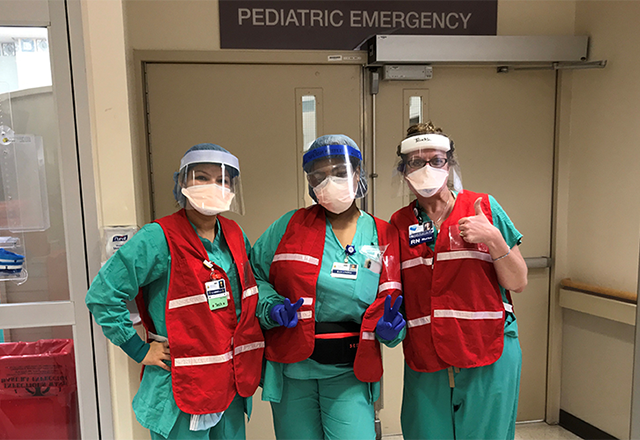
Click to enlarge. Image courtesy: Danielle Hirsch, Apr. 15, 2020Johns Hopkins All Children’s Hospital Ready to Help
Emergency center staff members at Johns Hopkins All Children’s Hospital wear protective equipment for the safety of patients and themselves during the COVID-19 pandemic.
Posted Apr. 24, 2020
“I help bring patients some peace.” — Aaron Mahomes
In normal times, drawing blood can produce anxiety for many patients. That apprehension is even higher now. “There’s a lot of fear that COVID-19 has produced, and part of my job now is calming those fears, reassuring the patients and letting them know they are in the right place to get the treatment they need,” says the Baltimore resident who has worked at the hospital for 11 months. “I help bring patients some peace.”
Posted Apr. 23, 2020
 Click to enlarge. Image courtesy: Raf Llinas, Image taken Apr. 12, 2020
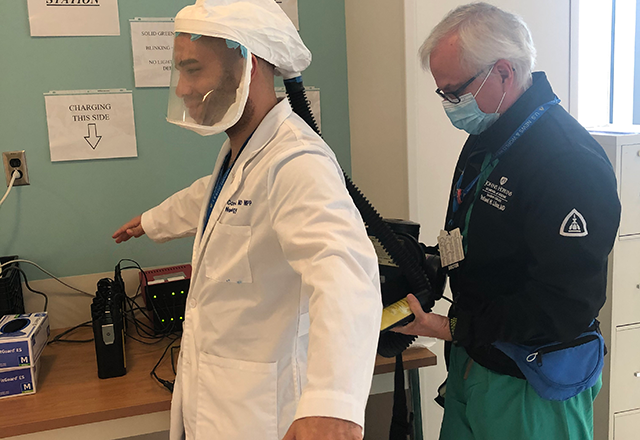
Click to enlarge. Image courtesy: Raf Llinas, Image taken Apr. 12, 2020A Resident Dons Equipment at Johns Hopkins Bayview Medical Center
Raf Llinas, M.D., director of neurology at Johns Hopkins Bayview Medical Center, helps School of Medicine resident Garret Conyers put on a powered air-purifying respirator as part of his personal protective equipment.
Posted Apr. 22, 2020
"There is a whole group of people behind the scenes working to support our front-line staff and patients.” — Marge Rodgers
Managing a crisis is part of the job for Marge Rodgers, administrator for orthopaedic surgery and physical medicine and rehabilitation at Johns Hopkins Bayview Medical Center. One of the challenges with COVID-19, says Rodgers, a member of the hospital’s rotating administrator-on-call team, is making sure to not neglect routine work.
“Right now, the hospital has many other patients,” says Rodgers, a resident of Baltimore’s North Roland Park neighborhood and a 17-year veteran at Johns Hopkins Bayview. “Last week we had 29 traumas because, for whatever reasons, people still wind up getting hurt.”
Posted Apr. 20, 2020
"I feel blessed to be part of a group that supports one another."
— Amy Penney
You can tell Amy Penney is smiling behind her mask. The charge nurse in the Progressive Care Unit at Suburban Hospital says that, during the COVID-19 crisis, her team is showing even more positive energy than usual. “Nurses are always striving to adapt and go with the challenges that come our way,” the Silver Spring, Maryland, resident observes. “Now that we’re seeing new variants of change — like policies and procedures — everyone's been gracious and willing to go with the flow, just like always. I feel blessed to be part of a group that supports one another.”
Posted Apr. 17, 2020
"I’m proud to provide essential care at home for our most vulnerable patients."
— Amy Kilen
Amy Kilen, a nurse practitioner with Johns Hopkins Home-Based Medicine, wears personal protective equipment (PPE), including a face mask and shield, gown and gloves, for her only in-person visit of the day. Before the COVID-19 pandemic, she visited several elderly, chronically ill patients in their homes each workday.
Now, because of the risk of infection, she “televisits” whenever possible. The Southeast Baltimore resident says she was reluctant at first to check up on patients remotely, but now looks forward to some aspects of these video visits. “Seeing your older patients on FaceTime is a neat intergenerational connection,” she says.
Posted Apr. 15, 2020
“Keeping people safe is my passion.”
— Dominick Metzger
Public safety is the calling for Dominick Metzger, a security officer at Suburban Hospital. “This is a very challenging time, but keeping people safe is my passion,” says the North Potomac resident and former U.S. Army military police officer. Metzger recalls that the morning this photo was taken, on April 3, was the same morning that Johns Hopkins Medicine instituted its universal masking protocol. “Many people coming to work hadn’t yet read the memo, or heard the news, so seeing us all wearing masks first thing as they came through the doors was a bit of a shock. Now it’s become routine.”
Posted Apr. 15, 2020
“There are constant challenges, and we have to think creatively.”
— Tina Hoang
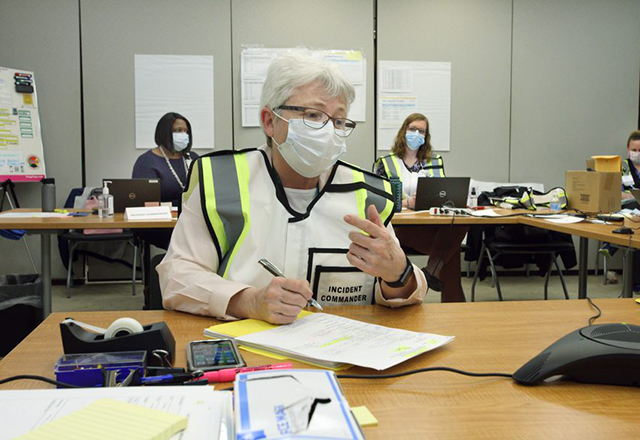
In the Command Center at Sibley Memorial Hospital, Tina Hoang looks up from her review of personal protective equipment protocols and explains her role.
Hoang, 33, has worked at Sibley for the past five years as an infection preventionist in the Department of Patient Safety and Quality. Her job — promoting strategies such as making sure clinicians wash their hands and get the proper personal protective equipment (PPE) training — kicked into high gear with the spread of the coronavirus that causes COVID-19.
“As we get surges of patients, we have to think creatively about where to place them and how to protect patients and staff,” she says. “I haven’t seen my office in quite some time. I’ve been living at the Command Center.”
Posted Apr. 15, 2020
Johns Hopkins Oncology Center OR
The Johns Hopkins Hospital team shares a message with the community.
Posted Apr. 6, 2020
Howard County General Hospital Pediatrics
Pediatric staff members at Howard County General Hospital wear protective equipment.
Posted Apr. 6, 2020
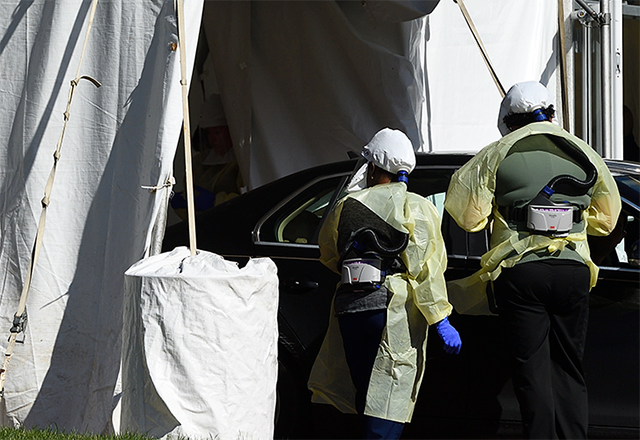
Johns Hopkins All Children’s Hospital
Johns Hopkins All Children’s Hospital staff members prepare for COVID-19 testing.
Posted Apr. 6, 2020
Johns Hopkins Coronavirus Test
Johns Hopkins microbiologists developed an in-house coronavirus test.
Posted Apr. 6, 2020
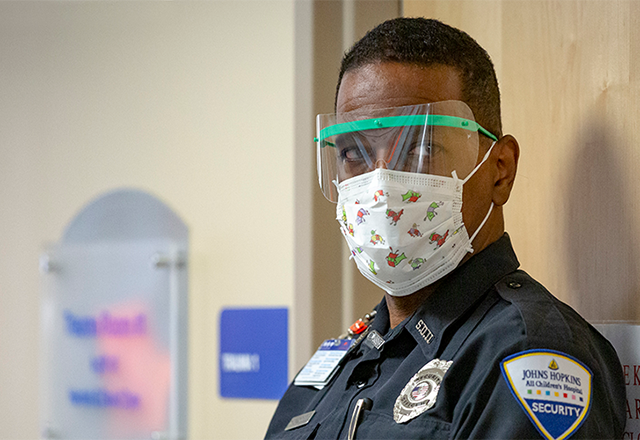
Johns Hopkins All Children's Hospital
A Johns Hopkins All Children’s Hospital security guard wears a kid-friendly mask.
Posted Apr. 6, 2020
Johns Hopkins Children’s Center
Johns Hopkins Children’s Center staff members share a message with kids.
Posted Apr. 6, 2020