Radical Prostatectomy
Procedure overview
What is a prostatectomy?
A prostatectomy is a surgical procedure for the partial or complete removal of the prostate. It may be performed to treat prostate cancer or benign prostatic hyperplasia.
A common surgical approach to prostatectomy includes making a surgical incision and removing the prostate gland (or part of it). This may be accomplished with either of two methods, the retropubic or suprapubic incision (lower abdomen), or a perineum incision (through the skin between the scrotum and the rectum).
Prior to having a prostatectomy, it's often necessary to have a prostate biopsy . Please see this procedure for additional information.

Prostate Cancer: Treatment Advances You Should Know About
Prostate cancer treatment has entered the robotics age. Using advanced robotic technology, Johns Hopkins surgeons can see the prostate in 3-D, magnifying everything 10 times. Johns Hopkins urologist Mohamad Allaf, M.D., explains what this means for patients, including fewer side effects.
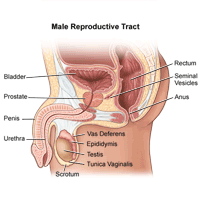
What is the prostate gland?
The prostate gland is about the size of a walnut and surrounds the neck of a man's bladder and urethra—the tube that carries urine from the bladder. It's partly muscular and partly glandular, with ducts opening into the prostatic portion of the urethra. It's made up of three lobes, a center lobe with one lobe on each side.
As part of the male reproductive system, the prostate gland's primary function is to secrete a slightly alkaline fluid that forms part of the seminal fluid (semen), a fluid that carries sperm. During male climax (orgasm), the muscular glands of the prostate help to propel the prostate fluid, in addition to sperm that was produced in the testicles, into the urethra. The semen then travels through the tip of the penis during ejaculation.
Researchers don't know all the functions of the prostate gland. However, the prostate gland plays an important role in both sexual and urinary function. It's common for the prostate gland to become enlarged as a man ages, and it's also likely for a man to encounter some type of prostate problem in his lifetime.
Many common problems that don't require a radical prostatectomy are associated with the prostate gland. These problems may occur in men of all ages and include:
-
Benign prostatic hyperplasia (BPH) . This is an age-related enlargement of the prostate that isn't malignant. BPH is the most common noncancerous prostate problem, occurring in most men by the time they reach their 60s. Symptoms are slow, interrupted, or weak urinary stream; urgency with leaking or dribbling; and frequent urination, especially at night. Although it isn't cancer, BPH symptoms are often similar to those of prostate cancer.
-
Prostatism. This involves decreased urinary force due to obstruction of flow through the prostate gland. The most common cause of prostatism is BPH.
-
Prostatitis. Prostatitis is inflammation or infection of the prostate gland characterized by discomfort, pain, frequent or infrequent urination, and, sometimes, fever.
-
Prostatalgia. This involves pain in the prostate gland, also called prostatodynia. It's frequently a symptom of prostatitis.
Cancer of the prostate is a common and serious health concern. According to the American Cancer Society, prostate cancer is the most common form of cancer in men older than age 50, and the third leading cause of death from cancer.
There are different ways to achieve the goal of removing the prostate gland when there's cancer. Methods of performing prostatectomy include:
-
Surgical removal includes a radical prostatectomy (RP), with either a retropubic or perineal approach. Radical prostatectomy is the removal of the entire prostate gland. Nerve-sparing surgical removal is important to preserve as much function as possible.
-
Transurethral resection of the prostate, or TURP, which also involves removal of part of the prostate gland, is an approach performed through the penis with an endoscope (small, flexible tube with a light and a lens on the end). This procedure doesn't cure prostate cancer but can remove the obstruction while the doctors plan for definitive treatment.
-
Laparoscopic surgery, done manually or by robot, is another method of removal of the prostate gland.
Are there different types of radical prostatectomy?
There are several methods of radical prostatectomy:
-
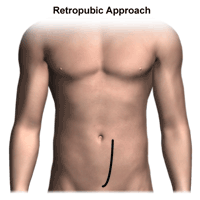
Radical prostatectomy with retropubic (suprapubic) approach. This is the most common surgical approach used by urologists (doctors who specialize in diseases and surgery of the urinary tract). If there's reason to believe the cancer has spread to the lymph nodes, the doctor will remove lymph nodes from around the prostate gland, in addition to the prostate gland. Cancer has spread beyond the prostate gland if it's found in the lymph nodes. If that's the case, then surgery may be discontinued, since it won't treat the cancer adequately. In this situation, additional treatments may be used.
-
Nerve-sparing prostatectomy approach. If the cancer is tangled with the nerves, it may not be possible to maintain the nerve function or structure. Sometimes nerves must be cut in order to remove the cancerous tissue. If both sides of the nerves are cut or removed, the man will be unable to have an erection. This won't improve over time (although there are interventions that may restore erectile function).
If only one side of the bundle of nerves is cut or removed, the man may have less erectile function, but will possibly have some function left. If neither nerve bundle is disturbed during surgery, function may remain normal. However, it sometimes takes months after surgery to know whether a full recovery will occur. This is because the nerves are handled during surgery and may not function properly for a while after the procedure. -
Laparoscopic radical prostatectomy. The surgeon makes several small cuts and long, thin tools are placed inside the cuts. The surgeon puts a thin tube with a video camera (laparoscope) inside one of the cuts and instruments through others. This helps the surgeon see inside during the procedure.
-
Robotic-assisted laparoscopic prostatectomy . Sometimes laparoscopic surgery is done using a robotic system. The surgeon moves the robotic arm while sitting at a computer monitor near the operating table. This procedure requires special equipment and training. Not every hospital can do robotic surgery.
-
Radical prostatectomy with perineal approach. Radical perineal prostatectomy is used less frequently than the retropubic approach. This is because the nerves can't be spared as easily, nor can lymph nodes be removed by using this surgical technique. However, this procedure takes less time and may be an option if the nerve-sparing approach isn't needed. This approach is also appropriate if lymph node removal isn't required. Perineal prostatectomy may be used if other medical conditions rule out using a retropubic approach.
With the retropubic approach, there is a smaller, hidden incision for an improved cosmetic effect. Also, major muscle groups are avoided. Therefore, there's generally less pain and recovery time.
Reasons for the procedure
The goal of radical prostatectomy is to remove all prostate cancer. RP is
used when the cancer is believed to be confined to the prostate gland.
During the procedure, the prostate gland and some tissue around the gland,
including the seminal vesicles, are removed. The seminal vesicles are the
two sacs that connect to the vas deferens (a tube running through the
testicles), and secrete semen.
Other less common reasons for radical prostatectomy include:
-
Inability to completely empty the bladder
-
Recurrent bleeding from the prostate
-
Bladder stones with prostate enlargement
-
Very slow urination
-
Increased pressure on the ureters and kidneys from urinary retention (called hydronephrosis)
There may be other reasons for your doctor to recommend a prostatectomy.
Risks of the procedure
As with any surgical procedure, certain complications can occur. Some possible complications of both the retropubic and perineal approaches to RP may include:
-
Urinary incontinence . Incontinence involves uncontrollable, involuntary leaking of urine, which may improve over time, even up to a year after surgery. This symptom may be worse if you're older than age 70 when the surgery is performed.
-
Urinary leakage or dribbling. This symptom is at its worst immediately after the surgery, and will usually improve over time.
-
Erectile dysfunction , also known as impotence. Recovery of sexual function may take up to two years after surgery and may not be complete. Nerve-sparing prostatectomy lessens the chance of impotence, but doesn't guarantee that it won't happen.
-
Sterility . RP cuts the connection between the testicles and the urethra and causes retrograde ejaculation. This results in a man being unable to provide sperm for a biological child. A man may be able to have an orgasm, but there will be no ejaculate. In other words, the orgasm is "dry."
-
Lymphedema. Lymphedema is a condition in which fluid accumulates in the soft tissues, resulting in swelling. Lymphedema may be caused by inflammation, obstruction, or removal of the lymph nodes during surgery. Although this complication is rare, if lymph nodes are removed during prostatectomy, fluid may accumulate in the legs or genital region over time. Pain and swelling result. Physical therapy is usually helpful in treating the effects of lymphedema.
-
Change in penis length. A small percentage of surgeries will result in a decrease in penis length.
Some risks associated with surgery and anesthesia in general include:
-
Reactions to medications, such as anesthesia
-
Difficulty with breathing
-
Bleeding
-
Infection
One risk associated with the retropubic approach is the potential for rectal injury, causing fecal incontinence or urgency.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Before the procedure
Some things you can expect before the procedure include:
-
Your doctor will explain the procedure to you and offer you the opportunity to ask any questions you might have about the procedure.
-
You'll be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something isn't clear.
-
In addition to a complete medical history, your doctor may perform a physical examination to ensure you're in good health before you undergo the procedure. You may also undergo blood tests and other diagnostic tests.
-
You'll be asked to fast for eight hours before the procedure, generally after midnight.
-
Notify your doctor if you're sensitive to or are allergic to any medications, latex, iodine, tape, contrast dyes, and anesthetic agents (local or general).
-
Notify your doctor of all medications (prescribed and over the counter) and herbal supplements that you're taking.
-
Notify your doctor if you have a history of bleeding disorders or if you're taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop these medications prior to the procedure.
-
If you smoke, you should stop smoking as soon as possible prior to the procedure in order to improve your chances for a successful recovery from surgery and to improve your overall health status.
-
You may receive a sedative prior to the procedure to help you relax.
-
Based on your medical condition, your doctor may request other specific preparation.
During the procedure
Radical prostatectomy requires a stay in the hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, a radical prostatectomy (retropubic or perineal approach) follows this process:
-
You'll be asked to remove any jewelry or other objects that may interfere with the procedure.
-
You'll be asked to remove your clothing and will be given a gown to wear.
-
You'll be asked to empty your bladder prior to the procedure.
-
An intravenous (IV) line will be started in your arm or hand.
-
If there is excessive hair at the surgical site, it may be clipped off.
-
The skin over the surgical site will be cleansed with an antiseptic solution.
-
The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
-
Once you're sedated, a breathing tube may be inserted through your throat into your lungs and you'll be connected to a ventilator, which will breathe for you during the surgery.
-
The doctor may choose regional anesthesia instead of general anesthesia. Regional anesthesia is medication delivered through an epidural (in the back) to numb the area to be operated on. You'll receive medication to help you relax and analgesic medication for pain relief. The doctor will determine which type of anesthesia is appropriate for your situation.
-
A catheter will be inserted into your bladder to drain urine.
Radical prostatectomy, retropubic or suprapubic approach
-
You'll be positioned on the operating table, lying on your back.
-
An incision will be made from below the navel (belly button) to the pubic region.
-
The doctor will usually perform a lymph node dissection first. The nerve bundles will be released carefully from the prostate gland and the urethra (narrow channel through which urine passes from the bladder out of the body) will be identified. The seminal vesicles may also be removed if necessary.
-
The prostate gland will be removed.
-
A drain will be inserted, usually in the right lower area of the incision.
Radical prostatectomy, perineal approach
-
You'll be placed in a supine (lying on your back) position in which the hips and knees will be fully bent with the legs spread apart and elevated with the feet resting on straps. Stirrups will be placed under your legs for support.
-
An upside-down, U-shaped incision will be made in the perineal area (between the scrotum and the anus).
-
The doctor will try to minimize any trauma to the nerve bundles in the prostate area.
-
The prostate gland and any abnormal-looking tissue in the surrounding area will be removed.
-
The seminal vesicles (a pair of pouch-like glands located on each side of the male urinary bladder that secrete seminal fluid and promote the movement of sperm through the urethra) may be removed if there's concern about abnormal tissue in the vesicles.
Procedure completion, both methods
-
The incisions will be sutured back together.
-
A sterile bandage or dressing will be applied.
-
You'll be transferred from the operating table to a bed, then taken to the post-anesthesia care unit.
After the procedure
After the procedure, you may be taken to the recovery room to be closely monitored. You'll be connected to monitors that will constantly display your heart beat (electrocardiogram—ECG or EKG) tracing, blood pressure, other pressure readings, breathing rate, and your oxygen level.
You may receive pain medication as needed, either by a nurse, or by administering it yourself through a device connected to your intravenous line.
Once you're awake and your condition has stabilized, you may start liquids to drink. Your diet may be gradually advanced to more solid foods as you're able to tolerate them.
The drain will generally be removed the day after surgery.
Your activity will be gradually increased as you get out of bed and walk around for longer periods of time.
The urinary catheter will stay in place upon discharge and for about one to three weeks after surgery. You'll be given instructions on how to care for your catheter at home.
Arrangements will be made for a follow-up visit with your doctor.
At home
Once you're home, it'll be important to keep the surgical area clean and dry. Your physician will give you specific bathing instructions. The sutures or surgical staples will be removed during a follow-up office visit, in the event they weren't removed before leaving the hospital.
The surgical incision may be tender or sore for several days after a prostatectomy. Take a pain reliever for soreness as recommended by your doctor.
You shouldn't drive until your doctor tells you to. Other activity restrictions may apply.
Once your catheter is removed, you'll probably have some leaking of urine. The length of time this occurs can vary.
Your doctor will give you suggestions for improving your bladder control. Over the next few months, you and your physician will be assessing any side effects and working to improve problems with erectile dysfunction.
Notify your physician to report any of the following:
-
Fever and/or chills
-
Redness, swelling, or bleeding or other drainage from the incision site
-
Increase in pain around the incision site
-
Inability to have a bowel movement
-
Inability to urinate once catheter is removed
Your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.



