Telemedicine: Catching Heart Problems Early
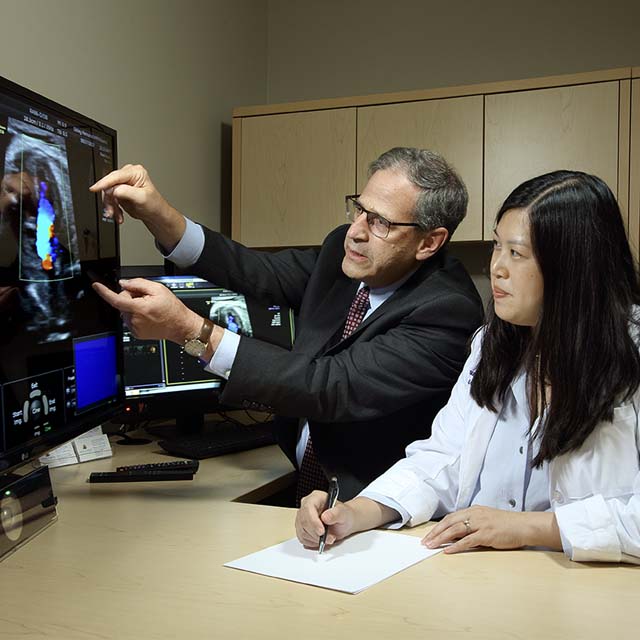
At Johns Hopkins Children’s Center in Baltimore, pediatric cardiologists Philip Spevak and Joanne Chiu assess blood flow in a fetal heart via real-time echocardiography imaging from Sibley Memorial Hospital in Washington, D.C.
Sibley Memorial Hospital obstetrician Rita Driggers was growing increasingly frustrated about delays in getting a follow-up echocardiogram by a pediatric cardiologist for expectant mothers whose sonogram indicated a possible cardiac problem. Visits from a pediatric cardiologist from an outside hospital 2 ½ days each month helped, but not enough. Driggers knew time was of the essence in having a detailed fetal echocardiogram performed by a physician trained in fetal cardiac evaluation.
“We do know the earlier the diagnosis is made the better the plan of care and the outcome,” says Driggers, medical director of maternal fetal medicine at Sibley.
The solution came in the form of a pilot telemedicine project initiated at Johns Hopkins Children’s Center, in which pediatric cardiologists Philip Spevak and Joanne Chiu direct and interpret echocardiograms from Baltimore with obstetric sonographers at Sibley, a Johns Hopkins Medicine affiliated hospital in Washington, D.C.
“We’re going to test this and see whether lack of physical presence is offset by the fact that we’re more able to support the program and be accessible,” says Spevak.
How does the project work? From a reading room in the pediatric cardiology suite at the Children’s Center, Spevak and Chiu, digitally and visually connected to a fetal echocardiogram machine and a sonographer at Sibley, join the exam. In real time, Spevak and Chiu see what the Sibley sonographer sees, allowing them to provide hands-on assistance in performing a fetal echocardiogram.
“Dr. Spevak can ask her to tweak the scan a little bit to the left so he can get exactly the images he wants,” says Driggers. “It’s like he’s doing the scan himself.”
If the study is normal, Spevak says, no personal telemedicine encounter with the family is necessary. If abnormal, Spevak or Chiu review the results face-to-face via video with the parents, who are in a comfortable consultation room at Sibley.
While being fully informed about a possible cardiac complication can be agonizing for parents, it is beneficial for parents in a variety of cases. Spevak explains that a mother with a prior pregnancy revealing hypoplastic left heart syndrome, for instance, wouldn’t have to wait 22 weeks to see whether her second child’s heart would be normal. In addition, an echocardiogram might expose a condition such as diaphragmatic hernia, where prenatal intervention is clearly beneficial. In almost all cases, Spevak stresses, parents are better prepared.
“If there’s structural heart disease, we can start the conversations with parents and connect them to the resources they need,” says Spevak. “They can meet with the cardiac surgeon and the neonatologist ahead of time and get a tour of the neonatal ICU. We can offer them the opportunity to talk to a family that’s been through what they’re going through.”
The Johns Hopkins imaging center for congenital heart disease supports 14 regional outreach clinics and 6 regional inpatient programs in Maryland through its remote telemedicine services.