Photo by Chiaki Kawajiri
Treating Addiction Without Judgment in East Baltimore
Twenty-five years ago, Michael Fingerhood began a medical practice that delivers dignified, first-rate primary health care to a population many physicians ignore.
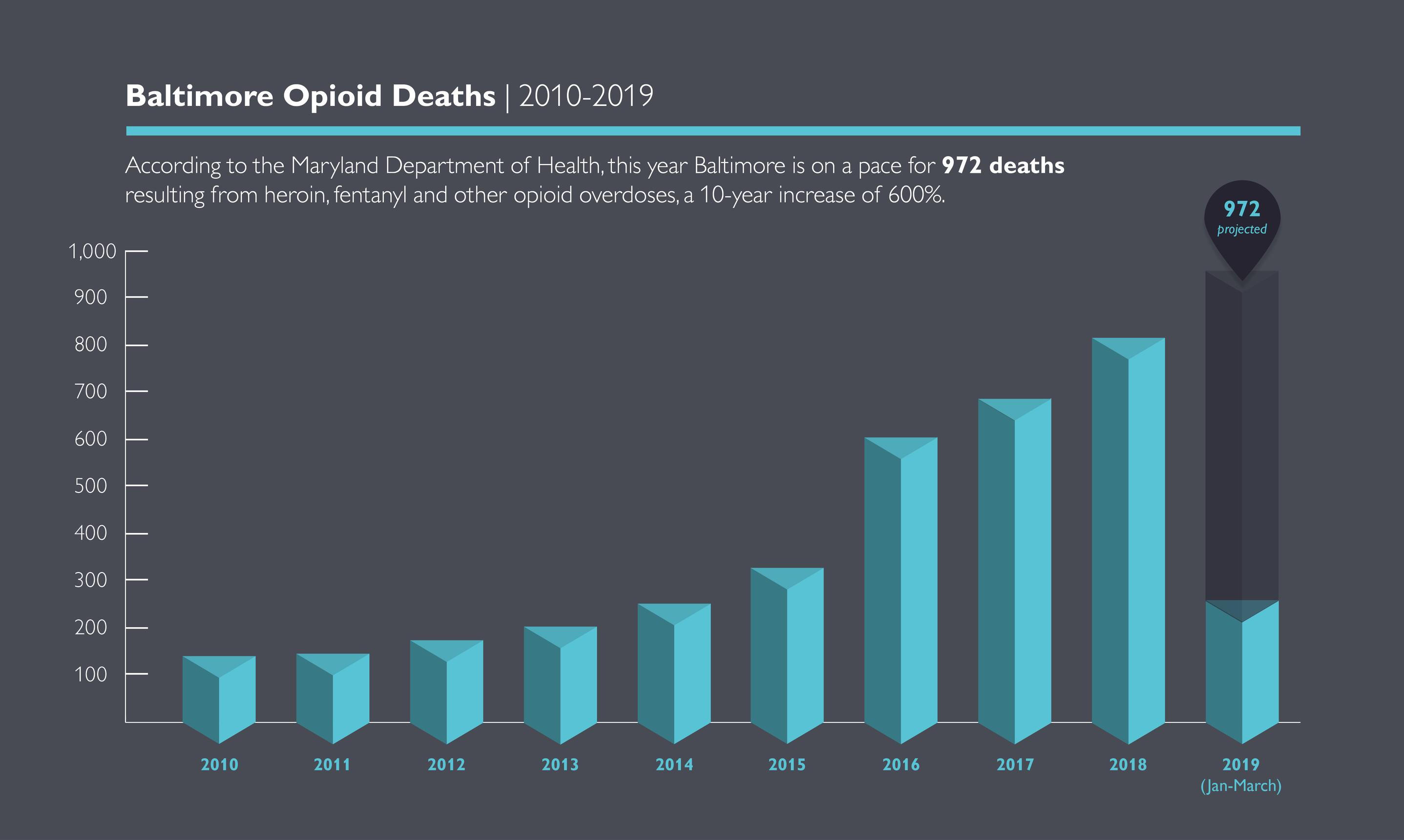
In 2017, 692 people died of opioid overdoses in Baltimore. One city resident says that number might have been 693 were it not for her doctor, Michael Fingerhood.
After years of recovery, the death of two close relatives left the woman reeling. She relapsed and overdosed on heroin seven times between June and August 2017. Several of those overdoses, she says, were nearly fatal.
“Dr. Fingerhood helped me through the most difficult time in my life,” says Amy Hudson (not her real name). “He just never gives up on me.”
The summer of 2019 marks the silver anniversary of the Comprehensive Care Practice at Johns Hopkins Bayview Medical Center, a primary-care clinic that places special emphasis on patients with substance use problems. Founded by Fingerhood at a time when many Baltimoreans struggling with addiction had few options for health care, the practice provides judgment-free support to people fighting dependence on drugs or alcohol.
Fingerhood says patients with substance use disorder need a special brand of primary health care.
“Addiction certainly doesn’t define the people who come to our practice,” he explains. “But it does need to inform the care we provide them.”
Heroin, fentanyl and other opioids are the most common substances Fingerhood and his team see, but the practice also treats patients with alcohol, cocaine and other substance use problems. More than 6,000 people, many of whom have been sober or off drugs for years, rely on the practice for routine medical care.
To schedule an appointment, call 410-550-2999.
“My sobriety is the first thing Dr. Fingerhood asks about when I see him,” says a longtime patient who battles alcoholism. “He’ll ask if I’m still going to my (Alcoholics Anonymous) meetings and talking to my sponsor. I haven’t used in almost 20 years, but it’s still something I have to pay attention to. Going to Dr. Fingerhood helps keep me grounded.”
FIGHTING FOR HIS PATIENTS
Fingerhood has dedicated a career to taking action against the disease of addiction, whether by chipping away at the crisis one patient at a time, by teaching Johns Hopkins medical students how to work with patients who have substance use disorders, or by advocating for sensible legislative policy.
In the early days of the prescription drug crisis, Fingerhood urged Maryland lawmakers to establish a database for physicians to check before prescribing narcotic pain medicine. That database, which is part of the Maryland Prescription Drug Monitoring Program, became state law in 2011.
Fingerhood serves on the board of the Behavioral Health Leadership Institute, a Baltimore nonprofit organization that operates a mobile treatment program and distributes anti-overdose medication around the city. With Darius Rastegar, another Johns Hopkins physician in the Comprehensive Care Practice, he co-authored the American Society of Addiction Medicine (ASAM) Handbook of Addiction Medicine, published in 2015 by Oxford University Press. In February of this year, the ASAM named Fingerhood a distinguished fellow.
Last December, Johns Hopkins alumnus and former New York City mayor Michael Bloomberg recognized Fingerhood as one of 10 “heroes” at a summit of the Bloomberg American Health Initiative, a project designed by the Johns Hopkins Bloomberg School of Public Health to address the environment, obesity, adolescent health risks, violence and drug abuse.
At the direction of Johns Hopkins University President Ron Daniels, Fingerhood and a team of five community leaders are guiding a quest to cut East Baltimore’s opioid addiction in half by 2024. A key component of that effort is to make medically assisted drug treatment available to anyone who needs it.
While there is no data to report yet, six months into the ambitious project, Fingerhood says he’s encouraged by the progress. “A lot of recent research says that access to buprenorphine is important when communities are fighting against opioids,” he says, referring to a prescription medication used to treat addiction.
The Substance Abuse and Mental Health Administration requires providers to obtain special certification to prescribe buprenorphine. As part of the plan he outlined with Daniels, Fingerhood has led an effort to get as many Bayview Medical Center physicians as possible to obtain that certification.
Fingerhood’s work is well respected around Bayview — his colleagues named him the hospital’s 2018 Physician of the Year — and around East Baltimore. As he strolls through the neighborhood that surrounds Patterson Park, one of his patients pops her head out the front door of her narrow row house and greets the doctor.
“Hey! I know you!” she hollers in a thick East Baltimore twang. Fingerhood smiles and waves.
“Hi. I’ll see you soon, right?” he asks her.
“You know you will!”
FROM BROOKLYN TO BALTIMORE
A bushy, light-gray mustache frames Fingerhood’s easy smile. He proudly declares he doesn’t own a white physician’s coat.
“For me, they just kind of create a barrier between me and patients,” he says. “Not my style.”
Born and raised in Brooklyn, New York, Fingerhood says he learned the importance of service and community from his parents, a teacher and a social worker who were active in their Flatbush neighborhood. Both sets of his grandparents immigrated to New York from Europe in the 1930s with very little money. His father’s family moved to a different Brooklyn apartment every 13 months for 20 years.
“If you signed a 12-month lease, you got a month free,” the physician explains, a trace of his Flatbush accent still intact.
Debbie Blunt, Comprehensive Care Practice administrator, has worked with Fingerhood since 1995 and says that, when the team moved to a new space this year, he insisted she take the largest office in the suite. “He said since I’m in my office a lot more than he’s in his, it makes sense,” she says. “I so appreciated that.”
A framed, black-and-white photograph of New York Yankees legends Mickey Mantle and Roger Maris hangs in Fingerhood’s office. Despite the pair’s combined 19 World Series appearances, Fingerhood insists that, in both baseball and life, he roots for the underdog.
“When I was a kid in New York, the Yanks were terrible,” he says, referring to an 11-year stretch of baseball futility in the Bronx. “I picked them up when they were at the bottom.”
Fingerhood traveled from Brooklyn to Baltimore to attend The Johns Hopkins University as an undergraduate. Then, after earning a medical degree from the Albert Einstein College of Medicine in New York, he returned to Johns Hopkins in 1986 for a medical residency.
In 1988, two years into the residency, Fingerhood began practicing the medicine that would ultimately become the basis for the Comprehensive Care Practice. The O’Donnell Heights Community Center, a 10-minute walk from Johns Hopkins Bayview Medical Center, housed indoor basketball courts, a Boys & Girls Club and, in its basement, a neighborhood medical clinic.
“Wow, was it hot in there,” recalls Theodore Parran Jr., who practiced alongside Fingerhood in O’Donnell Heights. Parran, now the chair of medical education at the Case Western Reserve University School of Medicine in Cleveland, remembers the clinic’s difficult conditions: “Very little air conditioning. We really cooked in those hot Baltimore summers.”
The building was tucked into a sprawling federally subsidized housing development, with barracks-style homes lining both sides of Gusryan Street on Baltimore City’s easternmost edge. Much of that housing has since been razed, but in Parran and Fingerhood’s years there, patients from the development packed the little clinic every weekday.
Along with help from a nurse practitioner, the two physicians treated all comers. “This was long before the Affordable Care Act, of course,” says Fingerhood. “In those days, Medicaid covered kids and pregnant women pretty well. But it didn’t do much for adults who didn’t happen to be pregnant.”
Thus, much of the care at the clinic was uncompensated. Parran remembers that the nurse practitioner would switch between adult medicine and pediatrics from one patient to the next. He also remembers the compassion Fingerhood showed.
“Mike treated every patient he saw like they were his friend,” says Parran. “I remember how genuinely pleased he was to see people, even if he knew he had to deliver some difficult news about that person’s condition. That has stuck with me, all these years later.”
Fingerhood says his time in O’Donnell Heights cemented his determination to work with a patient population that many health care providers ignore. A few years after his 1990 Johns Hopkins faculty appointment, he hatched the idea to start a primary care practice that would pay special attention to addiction.
The late Philip Zieve, then Bayview director of medicine, encouraged Fingerhood to pursue the venture with Ronald Peterson, who was the president of Bayview Medical Center at the time.
“Ron Peterson was a lot more supportive than I expected,” Fingerhood recalls. “He understood this community’s need for this kind of care.”
In June of 1994, the practice opened on the second floor of the center tower of the Mason F. Lord Building at Bayview. In addition to substance use problems, many of his early patients battled HIV and AIDS, which were the leading causes of death for Americans between ages 25 and 44. “The HIV epidemic was in full force,” Fingerhood remembers. “And, in those days, there wasn’t a lot we could do for patients after a certain point.”
Fingerhood and a nursing assistant staffed the practice alone for the first few months. “If the assistant was busy, I’d draw patients’ blood myself,” he recalls. Just as at the O’Donnell Heights clinic, most patients were uninsured and frequently had to pay out of pocket on sliding-fee scales. The hospital absorbed many of the costs.
“We started with about 500 patients,” says Fingerhood. “And we began growing pretty quickly.”
Today, the Comprehensive Care Practice has a bright, new space at Bayview to accommodate its 6,000-plus patients. “I think it’s important to offer care in an environment that’s dignified,” says Fingerhood. “Without it, the stigma that can accompany addiction just gets stronger.”
In addition to Fingerhood, the practice has four other physicians, three residents, a nurse practitioner, a physician’s assistant, a small administrative team and Blunt, who says nearly all Comprehensive Care Practice patients now have health insurance that pays for their care.
"I KNOW I CAN TELL HIM THE TRUTH"
“I’ve known Dr. Fingerhood for 14 years — maybe longer,” says Amy Hudson*, who hasn’t used heroin or crack for 20 months. “He’s honest with me and I’m always honest with him. When he asks me how I’m doing, I know I can tell him the truth.”
Hudson has a job and lives in a Baltimore County group home with others who are breaking free of addiction. She says the atmosphere of respect and trust at the Comprehensive Care Practice helped her form “a special bond” with Fingerhood.
In 2011, Hudson’s drug use was out of control, she says. Fingerhood told her she was no longer a candidate for buprenorphine, which is effective only when a patient is in active recovery.
“He can definitely be stern,” Hudson says. “Back in 2011, when I couldn’t stay off drugs, he told me ‘no more (buprenorphine). You need to be on methadone,’” a recovery drug that requires close supervision. (see sidebar)
Hudson’s recovery from that period was not without occasional relapses, she says. But she and Fingerhood have the kind of relationship in which Hudson knows she can be honest. “When I slip, I admit it. I tell him,” she says. “I trust him completely. He never, ever judges. He just says, ‘OK, Amy. Time to start over.’”
Removing the stigma that frequently accompanies substance use disorder is a priority for Fingerhood.
“It’s too easy to cast aside people who are poor or who have substance use disorders,” he says. “It happens to them just about everywhere else they go. But it doesn’t happen here.”

