Severely ill patients commonly experience impairments in physical function, mental health and cognition, which is collectively termed “post-hospital syndrome,” or “post-intensive care syndrome” (PICS) in the case of ICU survivors. Further, there are a growing number of COVID-19 survivors who were not hospitalized but have persistent symptoms, including shortness of breath, fatigue, headaches, palpitations and impairments in mental health and cognition. We recognize the need for a team approach to support the extraordinary number of COVID-19 survivors while driving care forward with comprehensive and standardized assessments, evidence-based approaches and the very best in patient-centered care.
The Johns Hopkins Post-Acute COVID-19 Team (JH PACT) Program is a collaboration between the Division of Pulmonary & Critical Care Medicine and the Department of Physical Medicine and Rehabilitation. Our goal is to provide interdisciplinary, standardized care to address the unique needs of COVID-19 survivors.
-
Physician Services
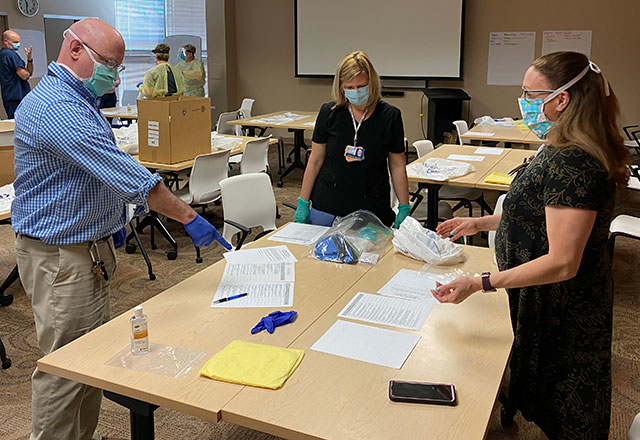
Our pulmonary and rehabilitation physicians conduct appointments via telemedicine or on campus.

-
Therapy Services
Our rehabilitation therapy services include physical, occupational, speech-language therapy and neuropsychology.
Important Notice on Referrals to JH PACT
Thank you for your referral. Due to the large influx of referrals to PACT Physical Medicine and Rehabilitation (PMR) for patients with predominant fatigue and dysautonomia symptoms, as of 11/12/2022 we are unable to accommodate any new referrals for JH PACT PMR at this time. Please check back periodically for updates.
JH PACT Pulmonology will continue to accept new patients with predominant pulmonary symptoms. Please use this form to refer to JH Pulmonary PACT.
- We recommend that the patient establish care with a primary care provider. Initial workup and management for common post-COVID conditions can be started by primary care. Review guidance on assessment and management of common post-COVID symptoms.
- If the patient is being referred for suspected autonomic dysfunction, consider referring to the Johns Hopkins POTS Program.
- If the patient is being referred primarily for fatigue, consider referrals to other local post-COVID clinics including COVID Recovery Program and Pediatric Post-COVID-19 Rehabilitation Clinic at the Kennedy Krieger Institute.
Resources for COVID-19 Survivors
- Johns Hopkins Outcomes After Critical Illness and Surgery (OACIS) research group: This site contains information and videos for patients, families, clinicians and researchers looking to learn more about recovering from a critical illness such as COVID-19.
- Education on post-intensive care syndrome: This handout from the American Thoracic Society provides an overview of (PICS).
- Pediatric Post-COVID-19 Rehabilitation Clinic: A clinic at Kennedy Krieger Institute for children and adolescents who have recovered from COVID-19 but need additional support to regain lost neurological and physical functioning as a result of the illness.
- Caring for Patients with COVID-19 and Post-Intensive Care Syndrome: This article lists some of the effects of severe COVID-19 and explains how we treat these symptoms at Johns Hopkins.
- Centro SOL: Spanish language resources for COVID-19 survivors. Centro SOL also hosts a weekly virtual support group.
JH PACT Research Studies
-
Summary: The goal of the COVID Patient Registry is to collect data on individuals who were diagnosed with COVID-19 and who are seen for follow up care at Johns Hopkins. We hope to understand the natural history of the illness and ultimately improve the care and survival of those who were treated for COVID-19 to improve understanding, treatment and survival.
P.I.: Ann Parker, M.D., Ph.D. Contact: [email protected]
-
Summary: People with solid organ transplants are at high risk of developing COVID-19, but the long-term neurocognitive aspects of COVID-19 infection (such as anosmia, loss of taste, loss of hearing, headaches, mental “fogginess,” confusion and fatigue) in this population is still not fully understood.
This study aims to: 1) Estimate the prevalence of mental, cognitive and physical impairments in solid organ transplant patients hospitalized with COVID-19 in the short-term and long-term period; and 2) understand changes in mental, cognitive and physical impairment in solid organ transplant patients hospitalized with COVID-19 in the long-term.
P.I.: Sami Alasfar, M.B.B.S., M.D. Contact: [email protected]
-
Summary: Recent data suggests that survivors of COVID-19 report adverse health status, including neurological and cognitive deficits and impaired pulmonary function, even months after discharge. Adult COVID-19 survivors after ICU stay are at higher risk of long-term disabilities and impaired quality of life. Post-hospitalization assessments are important to identify persistent deficits and stagnation in recover, since this may be amenable for early intervention and targeted rehabilitation.
This study aims to describe the health-related quality of life and the dynamics of neurologic and pulmonary dysfunction and recovery following intensive care admission for COVID-19. The study team will complete a baseline assessment of participants’ health prior to ICU admission, and then participants will complete a series of additional assessments (surveys, brain MRI, PFTs, chest x-ray, etc.) at three time points post-discharge.
P.I.: Sung-Min Cho, D.O., M.H.S. Contact: [email protected]
-
Summary: No studies of post-acute COVID-19 symptoms and sequelae have focused specifically on people living with HIV (PWH). Given elevated baseline levels of inflammation and T-cell activation in this population, we hypothesize that PWH are more likely to experience persistent symptoms after acute COVID-19 than HIV negative people.
This is part of a national study conducted remotely with telephone and online surveys and blood samples collected via a mobile phlebotomy company at the participant’s home. Specifically, this study aims to: 1) formally and prospectively characterize symptoms and sequelae of post-acute COVID-19 in PWH as compared to HIV-negative COVID-19 survivors and PWH and HIV-negative people with no history of COVID-19; and 2) identify blood-based biomarkers or immune signature(s) that associate with prolonged or persistent post-acute COVID-19 symptoms in PWH in comparison with the general population.
P.I.: Annie Antar, M.D., Ph.D. Contact: [email protected]
JH PACT in the News
- It's not just brain fog: Vertigo, hair loss, and lagging sex drive are also long COVID symptoms
- ‘A wake up call’: experts release new guidance on cardiovascular symptoms of long COVID
- How Long COVID Could Change the Way We Think About Disability
- For Patients with Long COVID, Chronic Fatigue Syndrome May Offer a Guiding Star
- In It For The Long Haul
- How Long-haul COVID Is Affecting Families Mentally and Emotionally
- EXPLAINER: What You Should Know About "Long Haul" COVID-19
- As the Pandemic in the US Slows, the Fight Against 'Long Haul' COVID Is On
- COVID Long-haulers: What We Know About the Debilitating Symptoms that Last for Months
- 'Long COVID' Impacting Patients Who Never Tested Positive for the Coronavirus
- Some COVID-19 Long Haulers Have Had Symptoms Since the First Wave. Can They Still Get Better?
- Maryland Man Battling 'Long COVID' for 11 Months
- ‘Dynasty’ Reunites To Fight Against Long COVID
- COVID-19 'Long-Haulers' Spark Area Health Care Movement to Create New Coronavirus Recovery Programs, Clinics
- Most Common COVID-19 Symptoms That Won't Go Away
- Who’s most at risk of developing long COVID? Experts think these 6 groups of people might be
- Physician Group Releases Guidance on Cardiovascular Issues in Long COVID
- The Long Haul
- COVID-19 Spreads As People Pass It Along to Someone They Live With
- Johns Hopkins Medicine Is Trying to Help COVID-19 Patients with Long-Term Symptoms
- Will Some COVID-19 Survivors Require a Lung Transplant to Fully Recover?
- Doctors: Most COVID-19 Patients Recover at Home
- Coronavirus Latest: Johns Hopkins Creates Team to Help COVID-19 Patients Deal with Psychological Effects of Virus
- Epic-Integrated Telehealth at Johns Hopkins Boosts Quality and Safety During Pandemic
- Johns Hopkins Doctor Talks Creative Approach Used to Assist Patients in COVID-19 Recovery
- Patients Treated for COVID-19 Now Coping with ‘Long COVID’
- As COVID-19 Cases Surpass Records, Cautions Against Holiday Gatherings
- Podcast: In It for the Long-Haulers—Investigating ‘Long COVID’