At Johns Hopkins Medicine, inclusive and equitable access to medical care and health information is a core value of our institution. Our care teams are working with community partners to give vaccines to our most vulnerable eligible residents, to provide access to COVID-19 testing, and to educate and inform our communities hardest hit by this pandemic.
Learning Resources
Toolkit for Community Organizations / Kit de herramientas para organizaciones comunitarias
Resources in English
At Johns Hopkins Medicine, we are collaborating with local partners to educate and inform our communities with facts about COVID vaccines. The downloadable resources below are for our community partners to print and share with the people and neighborhoods they serve, especially those with limited access to digital resources.
Recursos en español
Nosotros en Johns Hopkins Medicine estamos colaborando con socios a nivel local para educar a nuestras comunidades y brindarles información fidedigna sobre las vacunas contra la COVID-19. Los recursos a continuación, que pueden bajarse de Internet, son para que nuestros socios comunitarios los impriman y compartan con las personas y vecindarios a quienes sirven, especialmente aquellos que tienen acceso limitado a recursos en formato digital.
-
21224 COVID-19 Response Initiative
To respond to the major surge of COVID-19 infections in Baltimore’s 21224 area code, Johns Hopkins and the BUILD Organization joined forces to enact a robust and urgent containment and prevention strategy.

-
COVID-19 Community Education Task Force Report
The task force was formed in January 2021 to bring information about vaccine and COVID-19 safety to the Baltimore community. The task force, comprised of Johns Hopkins employees and allies, coordinated and developed dozens of events, campaigns and resources between January and September of 2021.

-
COVID-19 Anchor Strategy
The Workgroup identifies, develops and deploys interventions in coordination with the Baltimore school system, the city and state health departments, and other agencies and organizations to bring education, testing and other resources to Baltimore communities that are particularly hard hit by the pandemic.

-
COVID-19 Culturally Appropriate Care, Testing and Follow-up
Juntos seeks to reduce cultural and language isolation for Latinx patients and their families by connecting them with bilingual clinicians. Johns Hopkins clinicians are traveling to homeless shelters, sober living facilities and neighborhoods deemed COVID-19 hot spots to provide on-site testing.

-
After the 20-week Johns Hopkins-funded East Baltimore Food Access Initiative ended, the University partnered with Baltimore City and Saval Foodservices to continue delivering meals to families in East Baltimore. Through this partnership volunteers from local non-profits, community groups and faith-based organizations assisted with distributing meats, produce and dairy products to families impacted by COVID-19. In November and December, we provided 1,388,800 meals. In total from April to December 2020, we have provided 4,327,000 meals to local families.
Johns Hopkins has provided 200 food boxes per month to the NAACP through the East Baltimore Food Access Initiative since October.
-
New cases of COVID-19 have been on the rise in areas of Baltimore and state and local mandates were put in place to require mask use. It is critical that people living in Baltimore have access to masks and are encouraged to wear them.
Johns Hopkins procured a donation of 85,000 masks from the U.S. Department of Health and Human Services, Office of Preparedness and Response to meet the need.
The masks were 100% cotton, washable and reusable (up to 15 times), and packaged in sets of five. Hopkins tapped more than 60 local community and faith-based organizations to assist with the distribution including the NAACP, BUILD, The Door, Men and Families Center, Sister’s Together and Reaching, SECDC, The Mix Church and others.
Also, Baltimore Connect, through donations from Johns Hopkins Hospital, has distributed more than 15,000 to its member organizations for distribution in the local residents.
-
The economic effects of the COVID19 health crisis are widespread and the small business community has suffered tremendously. In response, the JHU Office of Economic Development is hosting a series of small business webinars and town halls that cover topics including:
- Returning to work safely
- Legal considerations for reopening
- And navigating the post COVID business world.
The Office of Economic Development has also produced an Entrepreneurship Matters webinar series that began in July. This series features topics and guests from a variety of industries including beauty, food, beverage, transportation, and real estate development.
-
JHU and JHM launched a four-part dialogue series about health, race, and social justice.
Series topics included:
- The 4th Amendment: Use, Misuse, and Case for Police Reform, August 20, 2020
- Protecting Our Youth: Confronting Society’s Role in the Harmonious Development of Adolescents, August 27, 2020
- Immigration Matters: Building Humanity Within a Fractured Immigration Landscape, September 10, 2020
- Decriminalizing Mental Illness: Empathetic Approaches to Mental Health Supports, September 24, 2020
- Road to Equity: Addressing Health Equity and Achieving Restorative Justice Symposium on October 8, 2020
-
Johns Hopkins office Government and Community Affairs has held briefings for state and local lawmakers about COVID-19 and health disparities and in coordination with the Anchor Strategy Workgroup held public health briefings for business leaders, faith leaders, and non-profit organizations, to disseminate public health information.
-
Johns Hopkins launched @JH Connects and the weekly JH Connects Newsletter to communicate JH programs, initiatives, and the impact to residents and elected officials. The @JH Connects social media has over 1,600 followers and the distribution list of the newsletter is approximately 3,000.
-
Since 2000, the Latino Health Initiative (LHI) of the Montgomery County Department of Health & Human Services (MCHHS) has been coordinating efforts in Montgomery County to improve the health outcomes of the Latinx community. Like other jurisdictions, COVID-19 has had a disparate impact on the Latino population in Montgomery County and the LHI has become the primary vehicle for addressing the pandemic in this community.
Johns Hopkins representative, Patricia Rios, MPH, serves on the steering committee for the LHI and ensures that Suburban Hospital is an active participant in the LHI’s programs, including a newly formed ad hoc “Latino Equity Workgroup” to more completely connect the population to available resources.
In August and October 2020, all of the Montgomery County hospitals – including Suburban – partnered with the LHI to assemble and distribute COVID-care kits to 10 partner agencies that serve the Latinx community. Suburban Hospital’s nursing professional development council assembled over 2,100 kits and delivered them to the agencies. The kits included masks, hand sanitizers, toiletries, and information about food support programs and other resources available through the LHI. There are plans for a future distribution of thermometers.
LHI also partnered with the hospitals and the Montgomery County Public Schools to sponsor a program in September to Spanish-speaking parents about the challenges of virtual learning. Suburban Hospital took the lead in planning the event by securing the panelists, designing the flyer, and promoting the program. event was offered on the Zoom and Facebook Live platforms and reached over 500 registered participants. It was subsequently shared and reported over 2,000 “views.” In November, there will be another community forum offered specifically to address the double threat of COVID-19 and influenza and to provide information about testing and share recommendations for timely treatment. This event will also highlight the need to get and availability of flu shots.
The COVID-19 crisis has also made existing food insecurity issues in Montgomery County worse. Suburban Hospital made a cash contribution to a new food distribution program started by a local church in Bethesda and will be conducting a food drive for two weeks in November among employees to gather donations for Manna Food Center’s “most needed” list.
-
Howard County General Hospital’s COVID-19 testing has been done in conjunction with our faith-based initiative called Journey 2 Better Health. We have partnered with congregations and sponsored and promoted community testing.
For those who have tested positive, we have reached out with our Community Care Team, a program of our Population Health Division, and provided supports such as food, medicine, follow up care, etc. when needed. We have tested nearly 3,000 county residents.
-
District of Columbia Housing Authority (DCHA) is proud to be working with Johns Hopkins Health System (JHSS) and Johns Hopkins Medicine (JHM), in partnership with D.C. Department of Health, to successfully vaccinate senior citizens living in DCHA properties in a pilot program.
-
During the first 120 days, Sibley Memorial Hospital's focus was to target resources for those hardest hit by the pandemic. Beyond protecting our frontline staff, Sibley collaborated with 27 partners who work in communities of color in Washington, D.C. and engaged 70+ Sibley staff members to support these efforts. For more information, contact [email protected].
-
The COVID-19 Public Private Taskforce is a partnership between the City of Baltimore, Johns Hopkins Medicine, CareFirst, and the University of Maryland Medical System to provide guidance for strategic decision making and resources allocation.
In the News
Stories from news media about Johns Hopkins Medicine’s work with the community to address equitable access to COVID-19 care and vaccines.
- Hopkins holds vaccine clinic at northeast Baltimore church, March 27, 2021
- Vaccination rollout ‘test’ could decide health chief’s confirmation says Md. Senate leader, March 27, 2021
- East Baltimore church hosts vaccine clinic focused on equity, March 26, 2021
- Todo lo que la comunidad latina debe saber sobre las vacunas contra el COVID-19 / Everything the Latino Community Should Know About COVID-19 Vaccines, March 3, 2021
- Baltimore Convention Center pilot program to vaccinate vulnerable populations, March 1, 2021
- Residents in certain city zip codes to be given preference for vaccine at Convention Center, March 1, 2021
- Baltimore Convention Center mass COVID vaccine site to prioritize vulnerable city residents amid criticism of inequity, March 1, 2021
- Partnering with churches, Maryland officials push pop-up clinics as way to address vaccine inequity, February 26, 2021
- Advocates working to get COVID-19 vaccine to Baltimore’s hard-hit Latino community, February 22, 2021
- How to Explain to Family That They Should Get the COVID-19 Vaccine, February 17, 2021
- Mobile clinics to deliver COVID-19 vaccines in Baltimore, February 8, 2021
Community Equity Stories
Johns Hopkins Medicine and community partners working together for vaccine and health equity.
-
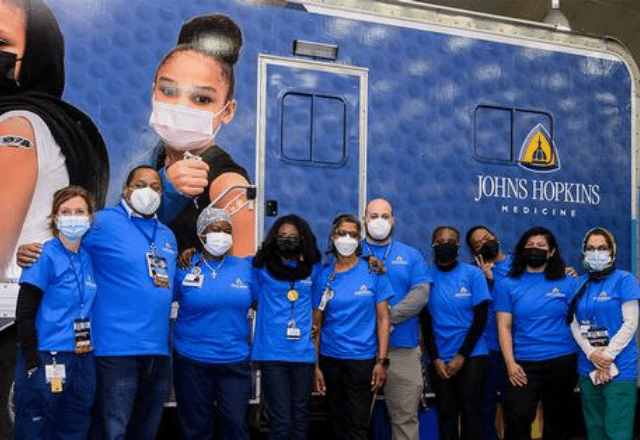
Watch: Delivering COVID-19 Vaccine Equity
June 8, 2021

-
Vaccine Prioritization Dashboard Launches for People with Disabilities
February, 16, 2021

-
Community Conversation Emphasizes Education and Trust
January 14, 2021

-
Johns Hopkins Takes COVID-19 Care to the Community
July 27, 2020

Additional Equity Stories
-
Published May 24, 2021

Johns Hopkins Medicine is dedicated to providing equitable care to all
Caring for neighboring communities is essential to the mission of Johns Hopkins Medicine (JHM). During the COVID-19 pandemic, JHM has strived to stay at the forefront of continuous changes in medicine and care options as they evolve, including by providing testing for the coronavirus that causes COVID-19, performing best practices to prevent the spread of illness, and offering innovative therapies, emotional support resources, language access options and, now, COVID-19 vaccines.
As the COVID-19 pandemic has made health disparities even more apparent, JHM knows that providing equitable access to care is incredibly important. As part of this effort, Johns Hopkins Medicine continues to develop new ways to offer access to information and services for all populations with a focus on those that are most vulnerable to the worst effects of the illness. It is important to meet community members where they live and to ensure that everyone who wants a vaccine can get one when supply is available.
“We need to make sure we continuously remove barriers that impede access to care, many of which have existed long before COVID-19, so everyone can get a vaccine,” says Sherita Golden M.D., M.H.S. “JHM is committed to building the trust of our community by collaborating with partnering organizations to reach populations that may not have the information they need about vaccines and the options available to them. Many people want to know what their pastor and neighbors think about the vaccine, and we need to work with our communities’ trusted messengers and arm them with information to help their communities.”
Initially, vaccine supply was extremely limited, and JHM had very little insight regarding how much vaccine it would receive on a weekly basis from the government. Considering these challenges, Johns Hopkins took a methodical approach to rolling out COVID-19 vaccine to communities.
As the pandemic progresses and government agencies continue to open COVID-19 vaccine eligibility to certain demographic groups, Johns Hopkins Medicine remains committed to providing services for its community and information about COVID-19 developments access to care.
Johns Hopkins Medicine has various partnerships and programs to reach its neighbors in nearby communities. For example, Maryland and Washington, D.C., providers collaborate with local governments to help vaccinate groups such as public-school employees. JHM is also going on-site to housing facilities for older people in Baltimore and Washington to vaccinate highly vulnerable residents in the comfort of their living spaces, which helps break down transportation challenges for those with mobility issues.
While mass vaccination options grow, many community members are best served by a community vaccination clinic due to language barriers and health and transportation challenges.
Johns Hopkins Medicine is conducting comprehensive vaccination clinics across Baltimore and Washington, in partnership with a variety of faith-based and homeless advocacy organizations, to equitably provide COVID-19 vaccines to the most vulnerable populations. JHM is also working closely with Latino community organizations, such as the Esperanza Center and Centro SOL, to make sure everyone who wants a vaccine can receive one without communication barriers.
“We know communities of color are being disproportionally impacted by COVID-19, “says Katie O’Conor, M.D., operations chief for Johns Hopkins Medicine’s unified command. “That’s why it is so important that we bring the vaccine to people in the neighborhoods where they live, and work with trusted community leaders to offer this as a welcoming option in a place where people feel safe and surrounded by their communities.”
A key barrier to seeking care is limited access to critical information. JHM has developed informative materials that are easily understandable by neighbors on all reading levels, translated them into several languages and distributed them among various communities. JHM also offers language access services, and printed materials and toolkits — particularly for vulnerable communities without access to digital communication.
Another important collaboration is with Mary’s Center that serves more than 60,000 minority community members. Over the next few months, JHM will connect this community with Johns Hopkins experts through Facebook, radio and television, so that health questions can be submitted by phone or mobile device and answered in real time. Mary’s Center also connects its members to JHM Espanol, the Johns Hopkins Medicine Spanish language portal, through its web homepage.
JHM has developed a new data tool — a vaccine prioritization dashboard — that helps people with disabilities determine when they qualify for the COVID-19 vaccine. The website, designed and run by researchers, students, and advocates for people with disabilities, aims not only to help the disabled community be informed and get vaccinated, but also to arm policymakers with data that can aid them in improving the health care system.
JHM collaboration spans community partners as well as fellow health care systems. Johns Hopkins is working with the state of Maryland and the University of Maryland Medical System to provide care at the Baltimore Convention Center field hospital. This care site, which was quickly mobilized very early in JHM’s pandemic response, is the city’s longest continually operating field hospital that offers COVID-19 testing, monoclonal antibody infusion therapy and vaccinations, as well as clinical care outside of a traditional hospital setting.
“It is critical to us to collaborate and use all the resources available to educate and reach all people about the dangers of COVID-19 and the importance of the vaccine,” says Gabor Kelen, M.D., director of the Johns Hopkins Office of Critical Event Preparedness and Response. “Diversity and equity are among our core values, and it is our responsibility to ensure we reach every member of the community in any way we can, to provide equitable access to health care and hope for the end of this pandemic.”
Johns Hopkins Medicine will continue to do everything possible to ensure that those who want and can get a COVID-19 vaccine have the opportunity to do so. Importantly, JHM wants to help reach people who don’t have the information they need to make a decision about getting the vaccine. It is JHM’s mission and privilege to serve its communities equitably and compassionately.
For more information about the COVID-19 vaccine, please visit the Johns Hopkins Medicine vaccine webpage here. For more information about health equity, please visit here.
Watch a video Johns Hopkins delivering COVID-19 vaccine equity
-
Published May 12, 2021 | Written by Vanessa Wasta
Imagine it’s your turn to receive a COVID-19 vaccine, but you have no reliable transportation, and it’s difficult for you to walk or to wait in line for long periods. Navigating the myriad vaccine registration websites is challenging, but for you, it’s impossible because you don’t have internet access.
The potentially life-saving vaccine is within reach, but to many Baltimore City residents, it seems unattainable. That’s why Johns Hopkins’ Katie O’Conor, M.D., Mobile/Community Vaccination Clinics director, and Jeanne Hitchcock, J.D., special adviser to the vice president for local government, community and corporate affairs, are leading efforts to bring vaccines to the doorsteps of the city’s most vulnerable residents.
“COVID-19 is disproportionately taking the lives of Black and Hispanic individuals in our communities, and we have to find ways to bring vaccines to them,” says O’Conor, a Baltimore native who leads a Johns Hopkins Medicine task force aiming to solve vaccine equity issues. “We’re employing a very focused approach to serve people of color and other marginalized communities in our city.”
Staff members and volunteers are setting up clinics at various city locations to provide COVID-19 vaccines to seniors and people with disabilities. O’Conor and her team start their day at 8:30 a.m., setting up a comprehensive clinic that is ready to vaccinate residents by 10 a.m. and that runs late into the day. They are ramping up to provide three or more clinics each week.
“Thank you for coming,” said a city resident at one of the program’s clinics. “We thought we had been forgotten.” O’Conor says this was a reminder to all those serving at the clinic that their work matters and is making a difference.
Some of the clinics are operated under a partnership with the Baltimore City Health Department and other health care partners. Soon, O’Conor will launch vaccination clinics at city faith-based organization sites, and infectious disease expert Kathleen Page, M.D., is setting up clinics in partnership with Hispanic communities and groups.
-
Story by Vanessa Wasta | Photography by Keith Weller
Follow along as Baltimore City community members receive their COVID-19 vaccinations from the Johns Hopkins Mobile/Community Vaccination Clinics team.
Welcome to the clinic

From left, community health worker José Jimenez, operations lead Benjamin Bigelow, and community health workers Karen Washington-Malone and Willetta Gombeh navigate clinic participants to each station and answer questions. The clinics are set up in community rooms at residential facilities or in large tents next to the facility, and staff members ensure that the space meets physical distancing guidelines.
Let’s sign you in

Baltimore resident Danny Lawrence, right, completes one of his first steps in getting a COVID-19 vaccine by signing in at a Johns Hopkins vaccination clinic with community health worker Willetta Gombeh.
Complete the registration

Administrator Saira Huggins, M.S., right, registers Charlie Billinger for a COVID-19 vaccine. Registration staff members collect demographic information from each participant to ensure that, overall, the clinics are serving populations that are hard hit by COVID and that have fewer opportunities to get vaccines. The participants receive an index card showing when they received the vaccine. Health care staff also talk with participants about informed consent and provide written materials about the vaccine.
Learn more about vaccination

School of nursing professor Nancy Glass, Ph.D., M.P.H., M.S., right, answers questions from clinic participant Hercules Williams. Clinic staff members answer questions about a wide range of subjects, including side effects, when immunity will start and when to get a second dose. The conversation topics often turn to life experiences. Senior residents often talk about their former jobs — some have been health care professionals, chefs and military personnel. Another popular topic among seniors is their grandkids, of course.
Vaccine is ready

Pharmacist Elizabeth Rodman, Pharm.D., M.H.A., draws a dose of COVID-19 vaccine from a vial. Ensuring that each clinic has the right number of vaccine doses is a complex process. There are 10 doses in each vial of this vaccine, and staff members need time to thaw the vaccines from subzero storage temperatures.
We’ll show you where to go

School of nursing professor Nancy Perrin, Ph.D., M.A., right, accompanies clinic participant Ellen Brown to her first station. Often, people are pre-scheduled for appointments at the vaccine clinics, but Johns Hopkins staff can vaccinate eligible walk-ins.
And answer your questions

Jenny Zhang, M.D., right, answers questions about the vaccine. When residents leave the clinic, primary care physicians and the Baltimore City Health Department can answer follow-up questions. Johns Hopkins Medicine will soon have a hotline for Baltimore City residents to call with vaccine questions.
Small sting!

Jenny Zhang, M.D., right, gives Ellen Brown a COVID-19 vaccine. Johns Hopkins Medicine plans to hold as many as three clinics per week at housing facilities for seniors and people with disabilities, and staff members are working with community organizations and associations to identify and vaccinate other community members who are eligible. Katie O’Conor says Johns Hopkins hopes to expand the clinics to faith-based organizations, schools, community organizations, homeless shelters and other locations to reach more people so that no one is left out. Each clinic can serve 100 to 150 people.
Making sure you feel well

Volunteer Anthony Evans, right, explains the vaccine index card to Vera Lee McKoy. After getting the vaccine, residents wait in an area near the clinic for 15 to 30 minutes to make sure they feel well and that their questions are answered before leaving the clinic.
Can’t come to the clinic?

Hooman Tadbiri, left, talks with Christine Freeland about her vaccine. For people with major mobility problems who can’t leave their apartment in the facility, a small team of Johns Hopkins health care staff members administers the vaccine at their apartment and monitors them for the 15 to 30 minute waiting period.
We bring vaccines to you!

Katie O’Conor says community residents are overwhelmingly eager to finally have the opportunity to get a COVID-19 vaccine at their doorstep, and those who are initially hesitant often opt to receive the vaccine after seeing their friends and neighbors safely vaccinated.
First dose complete

Christine Freeland’s first vaccine dose is complete, and she has one more to go. Clinic organizers do all they can to ensure that all of their vaccine doses are used, including knocking on residents’ doors to make sure that everyone who is eligible and wants a vaccine can get it. As residents sign in for their first dose of the COVID-19 vaccine, they receive a reminder card for the date and time that the Johns Hopkins team will come back to their building to give the second dose (if they are receiving the Moderna or Pfizer vaccine). Johns Hopkins Medicine health care teams and community partners follow up with every vaccine recipient to remind them of the date and time for their second dose. On the day of the second dose, team members go to each apartment in the building to remind anyone who may have forgotten their appointment. “It takes an exceptional number of volunteers to keep these clinics running, and we’re making a big impact in the lives of people receiving these vaccines,” says O’Conor.
Read more about COVID care and vaccine efforts in the community.
-
Published March 4, 2021

Johns Hopkins Medicine is committed to providing equitable care to all, while improving the health and wellness of our patients, personnel and residents in all our neighboring communities.
The COVID-19 pandemic has made existing health disparities even more apparent. In light of this concern, Johns Hopkins Medicine will continue to develop new ways to reach all populations — with specific consideration for vulnerable ones — to provide access to essential COVID-19 information and services. These include testing, care options, potential therapies, best practices to prevent the spread of illness, emotional support resources, language access options, and much more.
With highly effective vaccines now available to us in accordance with government supply distribution, we are focused on ensuring equitable access to COVID-19 vaccines for eligible populations. To help achieve this, Johns Hopkins Medicine has mobilized a multidisciplinary task force specifically focused on vaccine distribution, with equity and inclusion built into its foundation.
Through this task force, we continue to reach out to all of our patients, our neighboring communities and our personnel in many ways:
Efforts to Reach Our Patients
As government agencies continue to open vaccine eligibility to certain demographic groups, Johns Hopkins Medicine offers our patients information and access to resources through the MyChart electronic health record system, direct emails, our website, video content, social media, as well as through our health care providers and other referring physicians. Importantly, we ensure that we can reach our patients who may have limited computer or broadband access by providing a dedicated telephone call center that notifies patients of vaccine appointment availability. We also share information through local news and media outlets, as well as by sharing resources through community partner programs. We are committed to ensuring that our patients who want to be vaccinated receive the information they need — and, ultimately, the vaccine, as our supply allocations allow.

Outreach to Our Neighboring Communities
Johns Hopkins Medicine also has various partnerships and programs in place to reach our neighbors in nearby communities. For example, our Maryland and Washington, D.C., providers continue to collaborate with local governments to help vaccinate specific groups, such as public school employees. In addition, we are going onsite to various senior housing facilities to vaccinate these highly vulnerable residents where they live. We are also working closely with the University of Maryland Medical System to operate the Baltimore Convention Center Field Hospital, which offers COVID-19 testing, monoclonal antibody infusion therapy, vaccinations, as well as clinical care.
In addition, we have mobilized teams that are going out into the community to provide services, including testing and vaccinations within neighborhoods that have had high numbers of COVID-19 illnesses. In a collaborative effort between the Johns Hopkins Medicine Office of Diversity, Inclusion, and Health Equity, Johns Hopkins Medicine Language Services, and Centro Sol, a new pilot program — called Juntos — has helped to provide equitable resources to our Spanish-speaking inpatients with COVID-19. We are also leveraging well-established relationships with community and faith-based organizations to disseminate information about the vaccine.

Connecting with Our Personnel
Additionally, our health care systemwide Incident Command Center and our diversity councils are collaborating to reach our personnel across their various roles within the health care system to ensure that they have all the vaccine information and access they need. Just as with our patients, we are leveraging MyChart for vaccine appointment scheduling and notifications. To further enable this, we have established MyChart activation and support stations in our hospitals to ensure that those personnel whose work is not computer-based will receive assistance with securing appointments.
We have also established a special telephone line for personnel who lack computer access or who may experience technology challenges with accessing a vaccine appointment. Knowing that different personnel receive information in different ways, we have developed multiple means of communication — including signs, videos, infographics and a dedicated internal website, among other things — to help provide critical information to our staff.
At Johns Hopkins Medicine, we remain focused on creating effective and meaningful programs to ensure that our personnel, patients and neighboring communities feel they have the information and access they need to COVID-19 resources to remain informed and healthy.
For more information about COVID-19 and important resources. For more information about the COVID-19 vaccine.
-
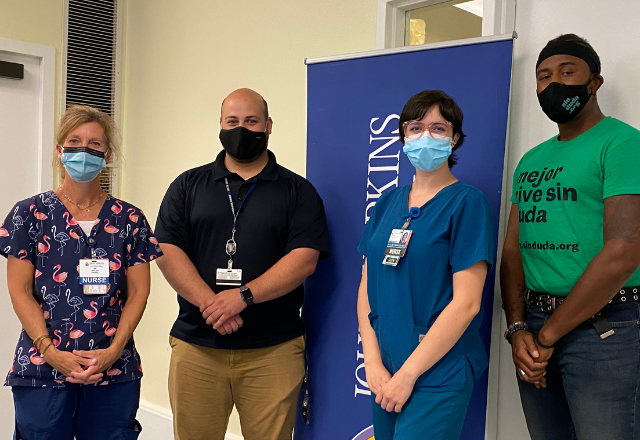
Published May 12, 2021

Johns Hopkins Medicine is dedicated to providing equitable care to all.
Throughout the COVID-19 pandemic, Johns Hopkins Medicine has focused on providing critical information and access to care for Latino community members, and, most recently, we have put enormous effort into offering the COVID-19 vaccine to our Latino neighbors in locations that are familiar and easy to access.
Initially, vaccine supply was extremely limited, and we had very little insight as to how much supply we would receive weekly from the government. Considering these challenges, we took a methodical approach to providing equitable access to the vaccine to vulnerable populations — with one area of focus being our Latino community members.
Johns Hopkins Medicine has identified limited English-proficient Latino patients as a vulnerable group at high risk for COVID-19. They may delay seeking care due to many issues, including demanding work schedules, language barriers, and concerns related to citizenship.
“COVID-19 has had a profound impact on communities of color,” says Kathleen Page M.D., an associate professor of medicine at the Johns Hopkins University School of Medicine and co-director of the health equity center Centro SOL. “The Latino community has been especially heavily hit. When I talk to these patients, they often tell me the same story. When everything shut down, they had to continue to work because they were essential workers. Many work in construction, the food industry or child care. Many had to keep working, because as undocumented immigrants they weren’t eligible for unemployment. This means that they had higher levels of exposure and also couldn’t always find the time to seek care if they did get sick.”
Through partnerships with Centro SOL and the Esperanza Center, a comprehensive Latino resource center, John Hopkins Medicine helps to promote health equity for Latinos in collaboration with faith and community organizations. Since June 2020, Johns Hopkins has run a coronavirus testing site at the Sacred Heart Church staffed by Spanish-speaking community health workers who register community members for testing and provide results over the phone to those who do not have internet access or who are undocumented.
If a community member has tested positive, the health workers refer them to resources such as food and cash assistance — or to shelter in a hotel, if needed — as part of the public-private partnership in which Johns Hopkins is an anchor institution. Patients without a primary care provider are also referred to the Johns Hopkins COVID-19 Ambulatory Response Team Clinic or to Spanish-speaking doctors who are part of Juntos, a collaborative effort between the Johns Hopkins Medicine Office of Diversity and Inclusion, JHM Language Services, and Centro SOL.
Community health workers also go out into local neighborhoods and talk about vaccine hesitancy and some of the reasons behind it. They answer questions about safety and myths, such as the misinformation that those who are tested or vaccinated are being reported to U.S. Immigration and Customs Enforcement. We have found that the Latino community is eager to get vaccinated but also afraid of the potential side effects of the vaccines. As such, we have partnered with the Esperanza Center to set up a COVID call-in line to answer questions and help people register for vaccination appointments, including at the pop-up Johns Hopkins vaccination clinic at the Sacred Heart Church.
Through visits with community members in locations where they spend their time, Johns Hopkins health workers have also conducted focus groups to gather information about the community’s needs. Our team has gone to local businesses such as beauty salons, restaurants and home improvement or construction businesses to ask people what they know about testing and the vaccine, and to hand out information pamphlets in Spanish.
“To access Latinos you need to go out on foot. People work all day long and do not know the available services,” says community health worker Alejandra Flores-Miller. “The ones that are hard to reach are those people who work at the construction sites, restaurants or those who clean, and they are exposed in their professions. Many are young but the risk is still very high because their living conditions are often crowded.
Johns Hopkins Medicine has also conducted town halls and forums in Spanish to talk about COVID-19. We launched a Spanish language web portal to consolidate and promote COVID-related content in Spanish. We are also working on a web-based toolkit that trusted community organizations can print out to share facts with their members.
In partnership with local health departments, our community health workers set up several pop-up vaccine clinics, including one at Sacred Heart of Jesus Church in Baltimore, which is located in the middle of a Latino neighborhood.
“We’re going outside the traditional walls of the hospital and meeting the community where they are,” says Ben Bigelow, acting associate director of operations for COVID vaccine administration. “We’ve built up a lot of trust in the community this way, since we’ve been doing it for more than a year.”
Johns Hopkins Medicine will continue to do everything possible to ensure those who want a vaccine have the opportunity to get one. The goal is to provide all of our neighbors with COVID facts, and vaccine information and access. It is our mission and privilege to serve all our communities equitably and compassionately.
For more information about the COVID-19 vaccine in Spanish, please visit our vaccine web page here. For more information about health equity, please visit our web page here.
-
Posted May 24, 2021

Johns Hopkins Medicine is committed to providing care for all patients
Care centered on the patient and the family is the foundation for what we do at Johns Hopkins Medicine. At all times, we are devoted to the highest level of service excellence and patient satisfaction. We strive to reduce patients’ anxiety, support families and address patient experience needs by developing new ideas for improving care and communication.
Throughout the course of the COVID-19 pandemic, Johns Hopkins has focused on providing critical information and access to care for its patients. Most recently, Johns Hopkins has put enormous effort into offering the COVID-19 vaccine to patients in a variety of ways.
Initially, vaccine supply was extremely limited, and there was very little insight as to how much supply would be received on a weekly basis from the government. Considering these challenges, a methodical approach was taken to provide the vaccine to patients with the supply available.
“We always knew that the final leg of this race would be the vaccine,” says Stephen Sisson, M.D., vice president of clinical operations for the Office of Johns Hopkins Physicians. “It’s part of Johns Hopkins’ mission that we do this the right way by making sure to distribute the vaccines in a way that’s representative of our patients.”
One element used to connect with patients is the MyChart electronic health record system, which documents patients’ health journeys and allows patients to see all of their health information in one place. The MyChart system enables Johns Hopkins to communicate with patients based on the information in their records and identify those who may be eligible for the vaccine. Importantly, patients can self-report on immunocompromised conditions or diagnoses that qualify them to be eligible to get the vaccine.
When vaccinations began, patients eligible to receive them were identified, and MyChart was leveraged to coordinate logistics for scheduling vaccine appointments using a computer-based randomized lottery process for the eligible group. Johns Hopkins also followed up via telephone calls, texts and emails to eligible patients, trying multiple avenues to alert people of their ability to receive the vaccine. As more vaccines became available, and as eligibility criteria expanded, self-scheduling in MyChart increased.
To help mitigate health care disparities and reach patients who have limited computer or broadband access, Johns Hopkins Medicine established telephone call centers that notify patients of vaccine appointment availability. The goal is to reach those without active MyChart accounts as well as high risk patient populations treated at Johns Hopkins affiliated community clinics. These clinics include:
- East Baltimore Medical Center
- John G. Bartlett Specialty Practice
- Johns Hopkins Outpatient Center 443-997-1875
- After Care Clinic
- Bayview Medical Center General Internal Medicine Center,
- Bayview Medical Center Comprehensive Care Practice,
- Esperanza Center
- Beacham Center for Geriatric Medicine at Johns Hopkins Bayview Medical Center
“Our patients are always so excited to receive the vaccine!” says Tanya Stamp, who works in the Johns Hopkins Outpatient Center and has been making personalized phone calls. “They say they’ve been trying to get on the lists everywhere and that they can’t wait to be able to leave their homes for this. I’m not a doctor or a first responder, but I feel like I’m helping because if I wasn’t calling them and reaching out to offer this opportunity, these are people who may not have gotten the vaccine. It just brightens my day that they’re so happy and thankful — this is why we do what we do at Johns Hopkins Medicine.”
As the pandemic progresses and government agencies open new phases of vaccine eligibility to different demographic groups, Johns Hopkins Medicine remains committed to informing patients about COVID-19 developments, access to care and resources. This is done in various ways, including with direct emails and video content, as well as through Johns Hopkins health care providers and referring physicians. The Johns Hopkins Medicine vaccine website and social media channels, where patients can access informative articles, infographics, answers to frequently asked questions and easy-to-use resources, are continually updated.
Johns Hopkins considers its patients’ unique needs. Many materials have been translated into several languages, and language access services are available. Messages are crafted to be easily understood by patients of all reading levels, and information is accessible outside of digital means — printable materials and toolkits can be shared with patients when they are onsite.
Community health workers collaborate with 2-1-1 Maryland to help patients when they need assistance making transportation arrangements. 2-1-1 Maryland provides Lyft rides to patients for vaccine appointments.
“Our team has been very successful reaching patients in this more personal way,” says Jamison Kies, M.H.A., clinical operations manager in the Division of General Internal Medicine. “Our staff is thrilled to be able to do this for our patients. They’ve felt empowered, and they continue to actively work to get patients scheduled when tickets are available. We realize the importance of catering our approach, and are seeing the impact of this work every day in our ability to reach and provide this care for our patients.”
Johns Hopkins Medicine is excited to provide life-saving vaccines to patients, and will continue to do everything it can to ensure that everyone can get one. Johns Hopkins is committed to reaching patients in a personalized way, and to making this and all processes as easy as possible while creating an environment that supports everyone in achieving the highest level of health.
For more information about patient care options during COVID-19, please visit the webpage here. For more information about the COVID-19 vaccine, please visit the vaccine webpage here.
-
Posted on May 24, 2021

Throughout the COVID-19 pandemic, Johns Hopkins Medicine has remained committed to reaching the most vulnerable patients and community residents with information, resources and care options.
“Johns Hopkins is a long-serving part of the communities in which we operate,” says Jeanne Hitchcock, special adviser to the vice president for Johns Hopkins local government, community and corporate affairs. “The well-being of our most vulnerable populations is a responsibility we take seriously, and we believe that responsibility dictates that we take our clinical services into the community to remove as many barriers to care as possible.”
In February, Baltimore City announced an effort to partner with area health care systems including Johns Hopkins Medicine, LifeBridge Health and MedStar Health to equitably bring COVID-19 vaccines to communities that have less access and greater challenges to getting vaccinated. Katie O’Conor, M.D. — Johns Hopkins Medicine’s unified command operations chief — and The Johns Hopkins University and Johns Hopkins Medicine Office of Government and Community Affairs worked together to assemble comprehensive, multidisciplinary vaccine teams.
Their efforts were aligned with and modeled after clinics launched by Sibley Memorial Hospital. Marissa McKeever, government and community affairs director; Nicki McCann, chief of staff; and Ben Bigelow, acting associate director of operations for COVID-19 vaccine administration, led the Sibley effort. The groups quickly mobilized to set up clinics at locations around Baltimore and Washington, D.C., in harder-hit communities determined by local governments. The robust teams include health care and logistical staff members, security personnel and other support professionals.
“We are reaching individuals that may have mobility issues or high-risk health conditions, and we’re working to meet them where they are,” says O’Conor. “We are dedicated to making an extra effort to make sure we’re providing equitable care to those that need it most.”
Dependent on the city’s guidance on these highest need areas, the Johns Hopkins government and community affairs team visits housing facilities, faith-based organizations, schools, community centers and other key locations to build relationships with community members. The teams identify language needs in advance, and they determine if any residents are home-limited — this helps the operational vaccine team plan, which can send a miniteam to vaccinate residents in their units.
The comprehensive vaccine team also uses the Office of Government and Community Affairs’ preliminary information to decide what it will need to bring on the day of the vaccine clinic. Each facility’s layout is assessed to establish a fluid flow of traffic and to keep everything moving as smoothly and efficiently as possible. The clinic’s structure and components are the same everywhere, but the layout is adaptable. These on-location clinics can be “popped up” and broken down in just a few hours.
Initially, vaccine supply was extremely limited, and Johns Hopkins had very little insight about how much supply it would receive weekly from the government. Considering these challenges, a methodical approach was taken to roll out the available supply to communities of older adults and people with disabilities, and to communities with significant barriers to care. Johns Hopkins continues to dedicate extra efforts to creating access for the hardest-hit and perhaps hardest-to-reach populations.
“Very similar to the senior community, the disability community has enormous barriers,” says O’Conor. “Many have mobility issues, health risks, or technology barriers to being able to register. Disabilities can be intellectual, developmental or physical, making getting to a clinic very complex, or not possible. We adjust as needed so residents don’t even need to go outside or put on a coat. They just go downstairs and get their vaccinations, or we go to them.”
The teams come prepared to accommodate everyone. O’Conor says the experience has been overwhelmingly positive, joyful and rewarding for the team.
While some people initially questioned getting vaccinated because they didn’t know how they would feel afterward, the team’s doctors answered all of their questions and gave them advice on possible symptoms. Language translators are also on-site to ensure clear and accurate communication. Once people saw others being vaccinated, they felt more confident.
“Johns Hopkins showed that they really care about my residents,” says Kimberley Moore, resident services coordinator at Johnston Square Apartments in Baltimore. “Too many residents have died from COVID in my building. I know the vaccine is not a cure, but it is something to help my residents fight it off. The team did a tremendous job. I’m looking forward to them coming back with the same energy, love and concern they showed the first time.”
Christine Freeland, an older adult who lives in Waters Towers Apartments, says she feels safer after getting the vaccine.
“I was afraid to travel without my shot,” says Freeland. “Once I get my second shot, I’m going to California to see my baby granddaughter for the first time. I’ve been encouraging all my friends to get the shot. When your time comes, go get it.”
For more information about the COVID-19 vaccine, please visit the Johns Hopkins Medicine vaccine webpage here. For more information about health equity, please visit the Johns Hopkins webpage here.
-
Published: May 24, 2021

Johns Hopkins Medicine is committed to providing vaccine information and access to all personnel
From the front lines to behind the scenes, Johns Hopkins Medicine’s diverse group of personnel has worked tirelessly to help inform, treat and protect our patients, visitors and colleagues during the COVID-19 pandemic. As essential members of the overall COVID-19 response, the staff members were among the first groups of people eligible to receive the vaccine, and Johns Hopkins quickly mobilized to administer vaccines to those who wanted them.
Initially, vaccine supply was extremely limited, and Johns Hopkins Medicine (JHM) had very little insight about how much it would receive on a weekly basis from the government. Considering these challenges, a methodical approach was taken to provide the vaccine to personnel with the supply available.
JHM, through the health care system-wide incident command center, and with the advice of various diversity councils and the scarce allocation committee, has continued to work diligently to reach personnel across their various roles to ensure that they have comprehensive vaccine information and access. MyChart, an electronic health record system, is leveraged. Initially, MyChart was used frequently to inform personnel when new vaccine appointments were available through a ticketing system. Now, with more available vaccine supply, personnel can self-schedule their vaccinations on MyChart.
To help encourage the use of MyChart by personnel who don’t have regular email access, MyChart activation and support stations were established in high traffic areas of facilities so that personnel whose work is not computer-based could get help securing appointments. These MyChart activation stations also offered an opportunity to learn more about the various roles colleagues play in this pandemic response, and those who staffed them offered encouragement and comradery.
“Some employees didn’t feel they were involved in direct patient care, and therefore shouldn’t get an early vaccine, so we helped them walk through the impact of their day-to-day work,” says Ebony Colina, an Epic applications supervisor and a member of the diversity council. Colina helped staff the MyChart stations. “We made sure to show everyone that each of us plays an important role that helps support the overall mission of delivering care. You are not ‘just’ a food services person. You’re an important part of enabling patient care, and every essential role matters.”
Johns Hopkins also held COVID-19 Vaccine Employee Zoom Town Halls, featuring Johns Hopkins expert physicians and other leaders. The town halls focused on issues that impact minority populations. Two were conducted in Spanish. Also, videos were created about vaccine equity and COVID-19 disparities, vaccine science and vaccine trial demographics, featuring minority physician leaders to help build trust about the vaccine and address areas of concern.
Personnel teams have widely different job responsibilities, from providing care for patients to ensuring the security of facilities and managing food services. Not all employees work behind a computer desk or are comfortable navigating technology. Knowing that personnel receive information in different ways, multiple means of communication were developed — including signs, infographics, a robust dedicated internal website with easy access to policies, data and guidelines, and other resources to help provide critical information to staff. One-page documents with QR codes that staff members could scan from their mobile devices provided weekly talking points for personnel during their regular shift meetings.
“We are incredibly grateful to our team that has worked tirelessly over the past year in response to the pandemic,” says Gabor Kelen, director of the Johns Hopkins Office of Critical Event Preparedness and Response. “And, we knew we needed to make an assertive effort to help address the issues amongst our personnel that were inhibitory toward being vaccinated, whether based in hesitancy or access. When there’s an entire group of our own personnel that doesn’t or can’t readily use our technology, it’s important to level the playing field and reach out to them in ways that fit within their daily routines.”
To help engage staff, Johns Hopkins Medicine connected with the leadership of environmental services, patient transport, food services, security, materials management, facilities, pharmacy, home care and supply chain, and offered leaders information to educate their staff members. Enthusiastic and well-informed personnel were appointed as health advocates and vaccine champions. They helped share messages about vaccine availability and the processes for getting vaccinated, as well as answer questions, during regular shift meetings.
As leaders continued to talk to personnel, they heard that it would be helpful for people to see colleagues they know get the vaccine. To accomplish this, and to demonstrate why staff members decided to get vaccinated, photo galleries and videos were developed that gave personnel the opportunity to speak personally and candidly about what the vaccine means to them and why they got vaccinated. The powerful videos were shared across the health care institution.
“It is critical to provide our personnel with up-to-date information, in ways they can access it within in their roles, so they can make an informed choice about their health care options,” says Carole Martens, director of facilities compliance for the health system. “We remain committed to ensuring that all of our essential team members know what COVID-19 resources, including vaccines, are available to them.”
Now that vaccines are more available, Johns Hopkins Medicine is creating pop-up and mobile clinics throughout the Johns Hopkins hospital system to reach personnel who have not received a vaccine. The Turner Auditorium vaccine clinic is also open for walk-in vaccinations on Thursdays and Fridays.
Johns Hopkins Medicine is excited to provide lifesaving vaccines to its personnel. And JHM will continue to do everything it can to ensure that those who want a vaccine can get one. All personnel deserve thanks for all they has done for Johns Hopkins’ patients, communities and, importantly, one another as we preserve through this pandemic.
For more information about JHM’s personnel outreach, visit the internal website here. For comprehensive information about COVID-19 vaccines, please visit here.